Could vagus nerve stimulation help ease pain from post-traumatic stress disorder (PTSD)? Functional MRI (fMRI) scans provided an affirmative answer by showing reduced activity in brain regions linked to pain processing in a study published online February 13 in PLOS One.
fMRI scans also showed how vagus nerve stimulation elicited a delayed response to pain among more than a dozen subjects who underwent the treatment.
"It's thought that people with certain differences in how their bodies -- their autonomic and sympathetic nervous systems -- process pain may be more susceptible to PTSD," said lead author Dr. Imanuel Lerman, an associate professor at University of California (UC) San Diego School of Medicine. "And so we wanted to know if we might be able to rewrite this 'misfiring' [through vagus nerve stimulation] as a means to manage pain, especially for people with PTSD."
The vagus nerve is located on both sides of the neck and extends from the brainstem to the abdomen. In recent years, imaging has been used to verify the efficacy of vagus nerve stimulation for a number of conditions. For example, researchers at Purdue University used MRI to track how well vagus nerve stimulation could alleviate stomach dysfunction, while French researchers used PET and electroencephalography to confirm how this stimulation helped to restore consciousness in a patient who had been comatose for 15 years.
In the current study, Lerman and colleagues used fMRI to examine 30 healthy study participants who had a heat stimulus applied to their legs. Half of the participants received noninvasive vagus nerve stimulation for two minutes via electrodes placed on the neck approximately 10 minutes before the heat stimulus. The other 15 subjects received a mock stimulation.
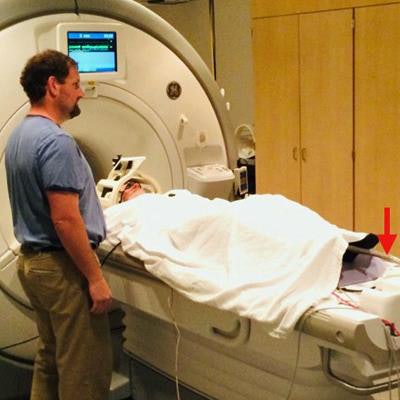
 A study participant undergoes an fMRI scan while heat stimulus is applied to his leg (red arrow). Image courtesy of UC San Diego Health.
A study participant undergoes an fMRI scan while heat stimulus is applied to his leg (red arrow). Image courtesy of UC San Diego Health.One measure of how the body's nervous system responds to pain is the amount of sweat on the skin. In this case, the researchers measured the sweat level of both groups before heat was applied and at several time points as the temperature increased.
They found that vagus nerve stimulation led to a reduced response to the heat stimulus in areas of the brain associated with sensory and discriminative pain processing, as well as emotional pain. The researchers also found a delayed pain response of approximately 10 seconds in those same brain regions among subjects pretreated with vagus nerve stimulation, compared with those who received the mock treatment.
Finally, vagus nerve stimulation prompted a decreased sweat reaction to the escalating heat stimulus among stimulated subjects, compared with those in the control group.
"Some people may need more vagus nerve stimulation than others to achieve the same outcomes and the necessary frequencies might change over time," Lerman noted.
The researchers plan to launch a clinical trial funded by the Veterans Affairs San Diego Healthcare System using military veterans with and without PTSD to determine to what degree, if any, vagus nerve stimulation can alleviate emotional pain and neural inflammation associated with PTSD.




















