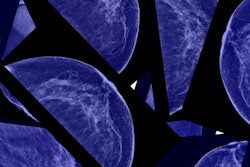
Apparent diffusion coefficient (ADC) values obtained from preoperative MRI with diffusion-weighted imaging (DWI) could help determine which women with breast cancer are at greater risk for developing metastasis, according to a study published online March 12 in Radiology.
South Korean researchers found a statistically significant difference between minimum and maximum in ADC values on MRI scans among women with distant metastasis compared with women with no distant metastasis. Women with invasive breast cancer also had a greater difference in axillary node metastasis, estrogen receptor negativity, and other key parameters, which in turn were associated with poor distant metastasis-free survival.
"Our results suggest that quantitative analysis of the ADC difference value as a marker of intratumoral heterogeneity could help identify a subgroup of women with breast cancer at elevated risk for developing distant metastasis," wrote lead author Dr. Jin You Kim and colleagues from Pusan National University Hospital in South Korea. "Identifying these patients could thereby potentially enable more personalized treatment plans and surveillance decisions."
DWI has become part of the regular routine to diagnose suspected breast cancer cases and characterize lesions with the help of ADC values. Previous studies have targeted multiple regions of interest to measure differences in ADC values and used those parameters as potential markers for assessing tumor aggressiveness and prognosis.
On the basis of those findings, the researchers hypothesized that the difference between minimum and maximum ADC values "could be useful to estimate the risk for distant metastasis." They decided, therefore, to investigate whether ADC parameters from preoperative DWI scans are associated with distant metastasis-free survival in patients with invasive breast cancer.
To test their hypothesis, Kim and colleagues reviewed medical records between June 2013 and June 2014 at their institution and found 258 consecutive women (mean age, 50.9 years ± 10.5; age range, 23-85 years) who met the study's inclusion criteria. The patients had newly diagnosed invasive breast cancer with core needle biopsy and had undergone preoperative MRI with DWI on a 3-tesla scanner (Magnetom Trio Tim, Siemens Healthineers) with a dedicated four-channel breast array coil. Distant metastasis-free survival was defined as the time from initial surgery to the date of breast cancer-specific distant metastasis.
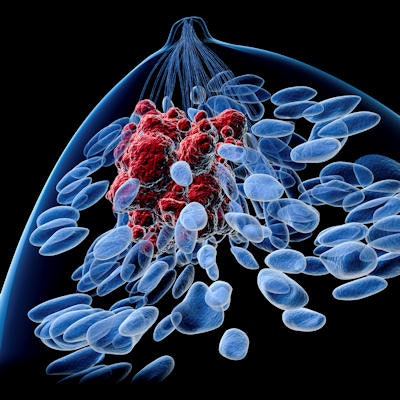
MR images showed an overall mean tumor size of 2.3 cm (± 1.5 cm) for all patients. The mean tumor size increased to 3.3 cm (± 2.0 cm) for the 25 patients (10%) who were found to have developed distant metastasis in bones, lungs, liver, and distal nodes. Among those women, 17 patients (64%) subsequently developed multiple distant metastases.
A further analysis of the DWI results found a statistically significant difference between minimum and maximum ADC values when comparing women with distant metastasis and those with no metastasis, as well significant differences between the two patient groups relative to axillary node involvement, lymphovascular invasion, estrogen receptor negativity, and HER2 positivity.
| Impact of ADC values in predicting distant metastasis from breast cancer | |||
| Patients with no distant metastasis | Patients with distant metastasis | p-value | |
| ADC difference* | 0.566 ± 0.187 | 0.743 ± 0.247 | < 0.001 |
| Axillary node involvement | 31% | 72% | < 0.001 |
| Lymphovascular invasion | 31% | 72% | < 0.001 |
| Estrogen receptor negativity | 23% | 48% | 0.007 |
| HER2 positivity | 36% | 60% | 0.02 |
"A higher ADC difference value obtained at preoperative DWI was associated with poorer distant metastasis-free survival in women with invasive breast cancer," the researchers wrote. "Intratumoral heterogeneity is a significant prognostic parameter and may be reflected in DWI and quantifiable by using ADC."