Add another clue for unraveling the mystery that is multiple sclerosis (MS). After using 7-tesla MRI to assess lesions in the brain's gray matter, researchers have found that the imaging technique could predict progression of the debilitating disease, according to a study published online April 9 in Radiology.
Led by senior author Dr. Caterina Mainero, PhD, of Massachusetts General Hospital in Boston, the researchers found that cortical lesions were located predominantly in grooves on the brain's surface, known as the sulci, and were associated with the degree of the subjects' deteriorated neurological condition. The study results would contradict previous conventional wisdom that MS is a white-matter disease, and, in the long run, they may help direct clinicians toward more effective MS therapies.
"Given that this accumulation is associated with progression of neurologic disability, its quantification might represent a useful tool for improving the monitoring of disease burden evolution," Mainero and colleagues wrote.
A white-matter disease
Mainero and colleagues have been involved in research for several years on the ability of 7-tesla MRI to visualize and detect in vivo lesions in the cortex of patients with MS. Their studies have included small cohorts of MS patients who underwent 7-tesla MR imaging to better evaluate cortical lesions in MS cases.
While MS has been considered a white-matter disease, more recent research has shown that lesions in the gray matter of the outer layer of the brain -- the cortical regions -- develop even earlier in the course of MS. The problem is that these abnormalities are not easily detected at lower field strengths such as 1.5 tesla and 3 tesla.
"White-matter lesions have been studied extensively in the past with MRI as part of the diagnosis and monitoring of MS," Mainero told AuntMinnie.com. "Neuropathological studies began to show about 10 years ago that the cortex is extensively involved by lesions during MS, but these lesions are very hard to see with lower-field clinical MRI protocols."
To better detect and locate the cortical lesions and how volume and location related to MS, the researchers recruited 20 patients with relapsing-remitting MS, 13 patients with secondary progressive MS, and 10 age-matched healthy controls between 2010 and 2016. Over a mean of 1.5 years (± 0.5 years), all of subjects underwent two MR imaging sessions within one week on 7- and 3-tesla MRI systems (Magnetom and TrioTim, respectively, Siemens Healthineers) using 32-channel head coils. The goal was to tally both the number of baseline cortical lesions and the development of new ones at follow-up. Subjects also were evaluated using the Expanded Disability Status Scale (EDSS) to determine the extent of their neurologic disability at the beginning of the study and at follow-up.
More cortical lesions
All 31 subjects were found to have at least one cortical lesion at baseline. At follow-up, all cortical lesions detected at baseline remained visible, with 25 (81%) subjects having at least one new cortical lesion per year.
In total, the researchers identified 93 new cortical lesions among these 25 patients: 30 new cortical lesions among relapsing-remitting MS patients and 63 new cortical lesions among secondary progressive MS patients. On average, more lesions (2.0 ± 2.8 per year) developed in the cortical region than in the brain's white matter (0.7 ± 0.6 per year). The difference was statistically significant (p = 0.01).
The total volume of cortical lesions was also a predictor of neurological disability at both baseline and follow-up assessment, based on EDSS results at both time points.
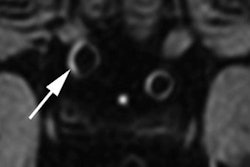
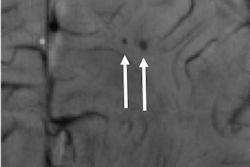
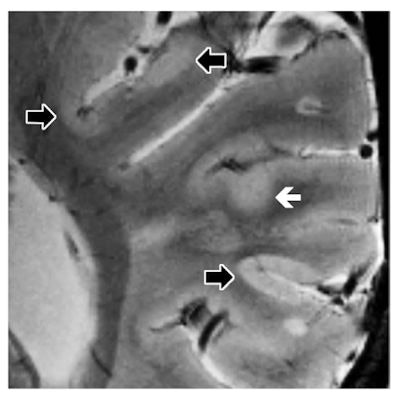
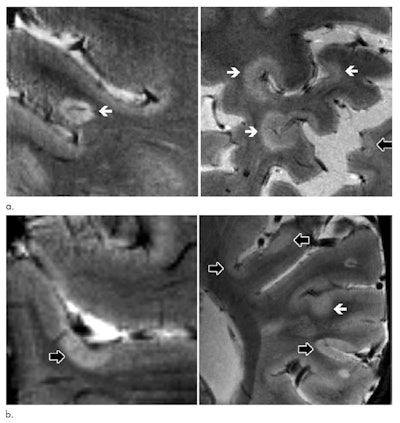 Axial 7-tesla T2-weighted images show examples of leukocortical lesions (white arrows) and intracortical lesions (black arrows) along with juxtacortical and periventricular white-matter lesions in different patients with MS. Images come from two different brain locations (a) in a 59-year-old man with secondary progressive MS (SPMS), and two different brain locations (b) in a 40-year-old woman with SPMS. Images courtesy of Radiology.
Axial 7-tesla T2-weighted images show examples of leukocortical lesions (white arrows) and intracortical lesions (black arrows) along with juxtacortical and periventricular white-matter lesions in different patients with MS. Images come from two different brain locations (a) in a 59-year-old man with secondary progressive MS (SPMS), and two different brain locations (b) in a 40-year-old woman with SPMS. Images courtesy of Radiology.The new cortical lesions were also primarily located in the sulci rather than in the gyri, which is the ridge on the surface of the brain. New cortical lesions in the sulci would indicate a possible link with an ongoing cerebrospinal fluid (CSF) neuroinflammatory process. While the researchers do not have an explanation for the accumulation of lesions in the sulci, the flow of CSF is likely to be restricted in the area, making the sulci more vulnerable to inflammatory responses.
Inflammation events
"These findings indicate that cortical lesions are likely driven by inflammatory events occurring in cerebral sulci, which previous neuropathologic examinations have reported as a preferential site of meningeal inflammation and possible restricted CSF flow with consequent stagnation of inflammatory soluble mediators," the authors wrote. "Our results also show that cortical lesion volume at baseline is related to EDSS progression independently from white-matter damage and cortical atrophy, highlighting the potential value of cortical lesion assessment at 7-tesla in the evaluation of progression of disease burden."
Mainero and colleagues plan to continue their research along this path. One target will be the issue of inflammation and how to "manage inflammation that we think is triggering cortical lesion development," she said. "We are also combining 7-tesla MRI with other imaging methods to look at the inflammatory cells that may be involved in this process."
The researchers also plan to expand their sample size to explore correlations between cortical lesion development and cognition, as well as some day monitoring the effect of therapeutic agents on the outcome of patients.