MONTREAL - MRI is a reliable way to validate changes in axillary lymph node volume and shape in situ in breast cancer patients after neoadjuvant chemotherapy, according to a study presented Monday at the International Society for Magnetic Resonance in Medicine (ISMRM) annual meeting.
Using 1.5-tesla MRI, the researchers confirmed significant reductions in nodal volume in patients who did and did not respond to therapy. In either case, MRI could be quite useful in monitoring cancer treatment on axillary lymph nodes and could help clinicians determine if changes are needed in patient management.
"We see that over time, postchemotherapy, both the nodes of the responders and nonresponders shrink significantly, whereas contralateral nodes start out small and end small," said lead study author Renee Faith Cattell, a graduate student at Stony Brook University in New York.
Size is everything
Measuring breast tumor volume is one method of determining the efficacy of neoadjuvant chemotherapy. Longitudinal monitoring of axillary lymph nodes is more challenging, but it remains important for prognosis and treatment planning.
Among the methods of assessing axillary lymph nodes are physical exam, or palpitation, and ultrasound. However, both approaches are limited to the detection of superficial lymph nodes and depend on the examiner's or operator's expertise. FDG-PET/CT also is an option, but the modality requires a radiotracer and has poor spatial resolution for micrometastases. The final choice is biopsy or dissection, each of which is quite invasive.
MRI, on the other hand, can offer 3D rendering of all lymph nodes -- rather than acquiring a single sample as done by biopsy -- and the modality is sensitive to changes in soft tissue. How effective is MRI for this clinical application?
"The goal of this study was to evaluate the longitudinal axillary lymph node morphological changes on MRI in response to neoadjuvant chemotherapy," Cattell told ISMRM attendees.
The researchers culled subjects from two different cohorts: 143 patients from the Investigation of Serial Studies to Predict Your Therapeutic Response with Imaging and Molecular Analysis (I-SPY1), which took place from 2002 to 2006 and used MRI to scan patients before, twice during, and after chemotherapy; and 71 patients from Stony Brook who underwent MRI before and after chemotherapy.
The number of nodes ranged from 62 to 80 between responders and nonresponders before and after therapy, respectively. The researchers defined responders as having no residual invasive nodal disease after neoadjuvant chemotherapy.
MRI findings
As one might expect, MR images showed a statistically significant reduction in the volume of ipsilateral nodes among patients who responded to neoadjuvant chemotherapy. Prior to treatment, the mean size of ipsilateral nodes was 2.33 (± 4.56) mL, compared with 0.45 (± 0.37) mL after therapy (p < 0.001).
Most interestingly, the volume of ipsilateral nodes also decreased significantly after treatment among patients who did not respond well to therapy. The mean volume was 2.58 (± 3.29) mL before treatment, compared with 0.77 (± 0.83) mL after neoadjuvant chemotherapy (p < 0.00001).
Neoadjuvant chemotherapy also affected the shape of the axillary lymph nodes among responders. While the axillary lymph node started out with the same shapely characteristics, over the course of the treatment, normal nodes and responder nodes expressed similar distribution. Nonresponder nodes, however, maintained irregular shapes.
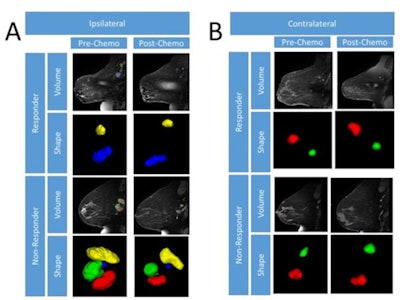 Representative MR images of ipsilateral (A) and contralateral (B) axillary lymph nodes modified in both size and shape before and after chemotherapy for a complete responder and nonresponder. Shape images are magnified to more easily see margins. Images courtesy of ISMRM.
Representative MR images of ipsilateral (A) and contralateral (B) axillary lymph nodes modified in both size and shape before and after chemotherapy for a complete responder and nonresponder. Shape images are magnified to more easily see margins. Images courtesy of ISMRM.Using the I-SPY1 dataset, the researchers also sought to determine if they could predict an outcome before, during, and after chemotherapy based on tumor volume and shape independently. They found that sensitivities ranged from 38% to 76%, and specificities varied from 36% to 89% along the three time points.
"We want to target an early time point, so we can tell a clinician early in treatment that these patients should be deviated from this sort of treatment and try something else that would be useful," Cattell said.
While the results are promising, there is still room for improvement. The researchers noted that current spatial resolution with MRI is 0.00098 mL per voxel. Given that some axillary lymph nodes are as small as 0.05 mL (55 voxels), they "cannot be quantified reliably. ... Future studies will need to increase spatial resolution to detect small nodes," according to the team.
Cattell and colleagues suggested that "more sophisticated approaches (texture analysis/optimized MRI sequences) should be explored to investigate normalization of shape and size features."