Using a "fast" MR technique instead of CT for imaging clinically stable pediatric patients with a suspected traumatic brain injury (TBI) can accurately diagnose them without sedation or exposure to radiation, according to a study published September 18 in Pediatrics.
Researchers did not need anesthesia to keep the children motionless during the fast MRI brain scan, which took a median imaging time of approximately six minutes. In fact, they were able to complete 95% of their scans. MRI achieved 90% compatibility with CT, which is known for its prowess in detecting skull fractures.
"These results suggest that fast MRI is a reasonable alternative to CT with the potential to eliminate ionizing radiation exposure for thousands of children each year," wrote lead author Dr. Daniel Lindberg, an associate professor of emergency medicine, and colleagues at the University of Colorado School of Medicine. "The ability to complete imaging in approximately six minutes, without the need for anesthesia or sedation, suggests that fast MRI is appropriate even in acute settings, where patient throughput is a priority."
Kids in the ED
Approximately 1.6 million children come to emergency departments (EDs) in the U.S. each year for suspected traumatic brain injuries. As many as 70% of those patients undergo a CT scan, which exposes them to ionizing radiation and potentially could increase their risk of cancer with repeated imaging. MRI uses no such radiation, but it does require the patient to lie still in the scanner bore for several minutes -- a task not easily accomplished by those younger than 6 years. Hence, sedation or anesthesia might be needed.
One alternative is fast MRI, which uses shortened "motion-tolerant" sequences to complete MRI brain scans without sedation, Lindberg and colleagues suggested.
"Some guidelines suggest that fast MRI could be used in young children with TBI, but it has not been shown to be as feasible or accurate as the current criterion standard of CT," they wrote. "Although small, retrospective comparisons of CT and fast MRI have reported limited sensitivity for fast MRI, most [studies] did not routinely use sequences that are most sensitive for blood products (e.g., gradient recall echo [GRE] and susceptibility weighted imaging). Our objective was to prospectively determine the feasibility and accuracy of fast MRI with GRE to identify radiographically apparent TBI in children < 6 years old."
Lindberg and colleagues prospectively recruited children between June 2015 and June 2018 from the emergency department at a level I pediatric trauma center. Subjects were eligible for the study if they were younger than 6 and had undergone a CT head scan during their emergency care. Subjects were excluded if they were clinically unstable or had a contraindication to MRI, a previous diagnosis of TBI, a structural brain lesion, or previous brain surgery.
Imaging protocols
CT scans (Somatom Definition Flash, Siemens Healthineers) included 3D image reconstruction of the skull. Fast MRI was performed on a 3-tesla scanner (Ingenia, Philips Healthcare), with sequences that included axial and sagittal T2-weighed single-shot turbo spin echo (TSE); axial T1-weighed turbo field echo; axial fluid-attenuated inversion recovery (FLAIR) single-shot TSE; axial gradient echo; and axial diffusion-weighted single-shot TSE planar imaging.
The researchers were able to complete 223 MRI scans (98%) on 225 subjects, with 215 patients (95%) doing so without sedation or anesthesia. The median time to complete MR imaging was 365 seconds (range, 340-392 seconds), compared with a median CT scan time of 59 seconds (range, 52-78 seconds). The median fast MRI time did not include patient screening, transport, positioning, and immobilization, as well as potential steps in the process that could lengthen imaging time.
"For research purposes, fast MRIs were independently interpreted by two of three pediatric radiologists [from the study] masked to all other clinical and imaging results and the initial clinical interpretations," the authors wrote. The trio achieved agreement of 96% on the presence of TBI among the 223 subjects who completed the fast MRI scans.
High sensitivity, specificity
As for the modalities' performance, CT identified TBI in 111 patients (50%), with the most common injuries being skull fracture (81 cases, 36%), subdural hematoma (27, 12%), and subarachnoid hemorrhage (24, 11%). Fast MRI identified TBI in 103 of the 111 CT cases and achieved sensitivity of 93% and specificity of 96%. MRI missed six patients with isolated skull fractures and two cases of subarachnoid hemorrhage.
"The majority of injuries missed by fast MRI were isolated, linear, nondepressed skull fractures," Lindberg and colleagues noted. "In the absence of associated brain injury or intracranial bleeding, skull fractures are rarely treated and generally do not require hospital admission."
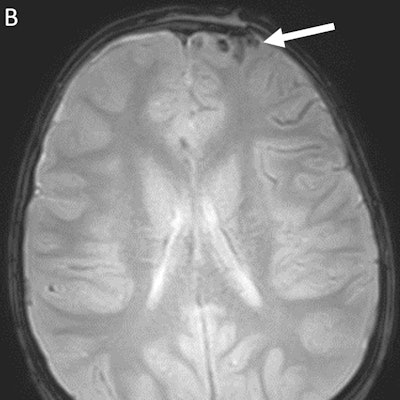
Conversely, fast MRI identified injuries in five patients that CT missed. Those injuries included three subdural hematomas, two parenchymal contusions, and one subarachnoid hemorrhage (one child had both a subdural hematoma and contusion).
 Axial nonenhanced CT (A) demonstrates no acute intracranial abnormality in a patient with left frontal calvarial fracture. Axial T2-weighted GRE MRI (B) reveals subarachnoid hemorrhage of the left frontal lobe (white arrow). Images courtesy of co-authors Drs. Daniel Lindberg and David Mirsky.
Axial nonenhanced CT (A) demonstrates no acute intracranial abnormality in a patient with left frontal calvarial fracture. Axial T2-weighted GRE MRI (B) reveals subarachnoid hemorrhage of the left frontal lobe (white arrow). Images courtesy of co-authors Drs. Daniel Lindberg and David Mirsky."Subjectively, radiologists felt that identification of skull fractures became easier over time with experience comparing CT with fast MRI," the authors wrote. "We recommend that fast MRI implementation begin with children who require repeat imaging for TBI identified by CT to provide a training period in which traumatic injuries can be compared on the two modalities."
Most-effective sequences
The most-effective MRI sequence for detecting TBI was GRE, which found signs of TBI in 94 patients, followed by T2-weighted single-shot TSE, which identified signs of TBI in 88 patients. The least-effective sequences were diffusion-weighted imaging, at 22 patients, and T1-weighted imaging, at 39 patients.
Lindberg and colleagues suggested that fast MRI could be used more often for pediatric patients with suspected TBI; however, they acknowledged that this might require additional staffing.
"Even at our referral center, fast MRI was not available for approximately one-quarter of consenting patients because of a lack of overnight staffing," they wrote. "Adding significant numbers of patients with trauma to busy MRI scanners without increased capacity could result in significant imaging delays, obviating the benefits of short imaging times and high completion rates."