MRI has a tendency to either overstage or understage disease in patients with recurrent prostate cancer after treatment, primarily due to the misinterpretation of fibrosis, according to a study published in the November issue of the American Journal of Roentgenology.
Researchers from China found that MRI did not accurately stage 22.8% of their subjects after chemoradiation therapy and excision. MRI findings also were exacerbated by inflammatory cell infiltration masquerading as residual tumors because the anomalies appeared as fibrotic areas on diffusion-weighted imaging (DWI).
"Mixed signal intensity on T2-weighted images or high signal intensity on DWI may be seen in patients with prostate cancer recurrence, leading to overestimation of residual tumor and underestimation of complete response," wrote the authors, led by Dr. Xiaoxuan Jia from Peking University People's Hospital (AJR, November 2019, Vol. 213:5, pp. 1081-1090). "Identification of the imaging features that lead to these misinterpretations could improve the accuracy of tumor response assessment."
Because of its high-resolution images, MRI is often the modality of choice for primary staging and restaging of prostate cancer after neoadjuvant chemoradiation therapy in patients with rectal cancer. While DWI improves sensitivity for detecting residual tumors, previous studies also have shown that tumor cells "may be partially or totally replaced by fibrosis and mucin," which can make differentiating between residual tumors and fibrosis more difficult, the authors noted.
To better gauge MRI's post-treatment proficiency, the researchers compared the modality's ability for accurate restaging in a retrospective analysis of 57 patients (median age, 62 years; range, 33-88 years) with stage III tumors or node-positive disease. Among the subjects, 43 patients (75.4%) received neoadjuvant chemoradiotherapy. All patients also underwent total mesorectal excision six to eight weeks later.
Both baseline and post-treatment restaging MRI exams were performed on the same 3-tesla scanner with a protocol that included sagittal T2-weighted fast-recovery fast spin-echo, coronal T2-weighted, and DWI. MR images and pathologic findings were compared for each case.
Jia and colleagues found that MRI correctly predicted tumor regression grade in 34 cases (59.6%), while the modality overstaged six patients (10.5%). Of those cases, three patients (50%) had severe edema of the mucosa and submucosa adjacent to the tumor, which was misinterpreted as residual tumor. In two patients (33.3%), the muscular layer next to fibrotic area appeared as intermediate signal intensity on T2-weighted images and was misinterpreted as residual tumor. The sixth patient was misdiagnosed with a diagnosis of mucinous adenocarcinoma.
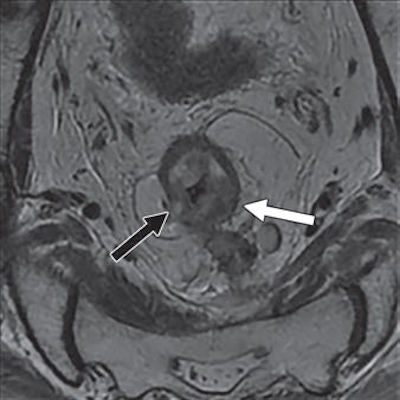
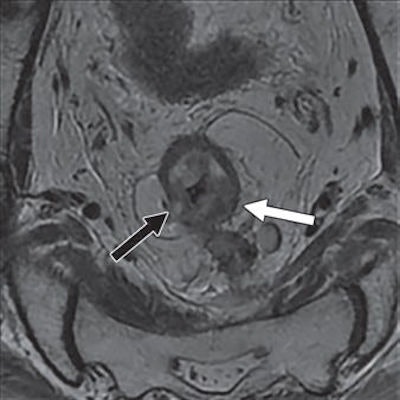 Above: Restaging oblique axial T2-weighted MR image shows small area of high signal intensity (black arrow) within intermediate signal intensity of primary tumor (white arrow), which was interpreted as acellular mucin and tumor regression grade 4. Below: A histologic slice, however, shows only a small number of tumor cells (black arrowheads) scattered in massive fibrosis (white arrowheads) and acellular mucin (arrow). The disease was reclassified as pathologic tumor regression grade 2. Images courtesy of AJR.
Above: Restaging oblique axial T2-weighted MR image shows small area of high signal intensity (black arrow) within intermediate signal intensity of primary tumor (white arrow), which was interpreted as acellular mucin and tumor regression grade 4. Below: A histologic slice, however, shows only a small number of tumor cells (black arrowheads) scattered in massive fibrosis (white arrowheads) and acellular mucin (arrow). The disease was reclassified as pathologic tumor regression grade 2. Images courtesy of AJR.The researchers also found that fibrosis "could manifest as a shape and signal intensity similar to the shape and signal intensity of invaded vessels that shrank after treatment. This result was especially evident in vessels with a diameter smaller than 3 mm.
Conversely, MRI understaged seven patients' (12.3%) tumor regression grades. In all cases, the patients had their post-treatment tumor regression grade of 3 mistakenly classified as grade 2 due to fibrosis in the tumor area.
"In cases of understaged disease, we found that the scattered tumor cells in fibrotic areas were not accurately identified at MRI," the authors wrote. "Similarly, micrometastasis within lymph nodes could not be accurately identified on MR images, even when signal intensity on diffusion-weighted images was considered. Using a slice thickness of at least 3 mm may have also led to the omission of small positive lymph nodes."




















