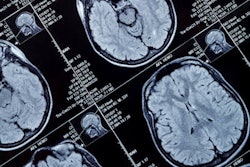
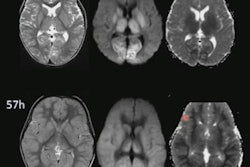
Lesions that appear on diffusion-weighted imaging (DWI) MRI scans represent acute sequelae of chronic cerebral small-vessel disease, according to a July 20 study in JAMA Neurology. In addition, the presence of DWI lesions signifies worse prognosis after intracerebral hemorrhage (ICH), mainly for deep hemorrhages.
A research team led by Dr. Santosh Murthy at the Clinical and Translational Neuroscience Unit of Weill Cornell Medicine in New York City pooled individual patient data from three randomized clinical trials and one multicenter prospective study. Doing so, they were able to investigate DWI lesions and factors associated with them.
"In this individual patient data meta-analysis of more than 1,700 patients with ICH and MRI scans, younger age, Black race, acute blood pressure elevation, radiological markers of small-vessel disease, and admission hematoma volume were associated with DWI lesions after ICH," the authors wrote. "Diffusion-weighted imaging lesions were independently associated with poor ICH outcomes in patients with deep ICH but not lobar ICH."
Why look at DWI lesions?
Potentially covert brain infarcts identified via DWI-MRI in patients with acute ICH occur more frequently than apparent ischemic strokes -- from 15% to 41%. Several studies have addressed the relationship between ICH and DWI lesions, but a large knowledge gap in the understanding of the downstream effects of acute ICH and DWI etiology remains.
Murthy and colleagues explored factors associated with DWI lesions and hypothesized that biological pathways determining DWI lesions may differ between deep and lobar ICHs. They also posited DWI lesions have a location-specific influence on ICH outcomes.
They culled data from the Minimally Invasive Surgery Plus Alteplase for Intracerebral Hemorrhage Evacuation phase III trial, Antihypertensive Treatment of Acute Cerebral Hemorrhage trial, Intracerebral Hemorrhage Deferoxamine phase II trial, and the multicenter prospective study Ethnic/Racial Variations of Intracerebral Hemorrhage. After exclusions, 1,752 patients with brain MRI scans were identified: 619 with lobar ICH, 972 with deep ICH, and 161 with brainstem or cerebellar ICH.
The research team found lesions appearing on DWI scans in 549 patients. The factors associated with these lesions in multivariable regression models were the following:
- Younger age
- Black race
- Admission systolic blood pressure
- Baseline hematoma volume
- Cerebral microbleeds
- Leukoaraiosis
The group also found DWI lesions were independently associated with a poor modified Rankin score, a measure of neurological disability. However, DWI lesions were not associated with mortality. In subgroup analyses, similar factors (i.e., admission hematoma volume, cerebral microbleeds, etc.) were associated with DWI lesions in lobar and deep ICH.
In lobar ICH patients, DWI lesions were not connected with mortality. In deep ICH patients, DWI lesions correlated to a modified Rankin score of 4 to 6, but again, not mortality.
"Our results confirm that neuroimaging markers of small-vessel disease such as cerebral microbleeds and leukoaraiosis are associated with DWI lesions," the researchers wrote. "The association between Black race and DWI lesions noted in our analysis may also be attributable to a greater burden of subclinical cerebrovascular disease among Black participants compared with those of other races, including a higher prevalence of vascular risk factors and differences in genetic susceptibility."
They also found the burden of high blood pressure alleles was related to larger hematoma volumes and worse ICH outcomes, which implies small-vessel disease and hematoma size may share a similar genetic predisposition.
"Therefore, DWI lesions may be surrogate markers for chronic hypertensive arteriopathy," they added.