Many more patients with implanted devices like pacemakers could safely undergo MRI and reap clinical benefits of the modality than do so currently, according to a new registry study published in Radiology: Cardiothoracic Imaging online October 22.
The prospective Patient Registry of Magnetic Resonance Imaging in Non-Approved Devices (PROMeNADe) registry study tracked experiences of more than 500 patients with implanted devices who underwent MRI -- including thoracic studies. The researchers found no complications and plenty of upside for patient care.
The results suggest the potential for broader use of MRI in patients with implanted devices -- such as pacemakers and implantable cardioverter defibrillators (ICDs) -- that are "non-MRI conditional," meaning they do not meet the safety criteria of the U.S. Food and Drug Administration (FDA).
In particular, the data support the use of MRI in three important populations with non-MRI-conditional devices who may currently be excluded due to safety concerns:
- Those who need thoracic MRI
- Those who are pacemaker-dependent with ICDs
- Those who have fragmented or abandoned leads (wires that connect a device to the heart)
"This study adds to the growing literature demonstrating that MRI examinations can be performed safely in patients who have non-MRI-conditional devices; this finding may prompt more institutions to start offering MRI examinations to these patients," Dr. Sanjaya Gupta, an electrophysiologist at Saint Luke's Mid America Heart Institute in Kansas City, MO, and colleagues wrote in Radiology: Cardiothoracic Imaging.
Furthermore, Gupta suggested in a statement from the RSNA that the registry data could also support an expansion of FDA-approved indications for MRI-compatible devices.
The study was conducted to fill a gap in the literature and practice about MRI safety in patients with implantable cardiac devices. Imaging studies may be performed on patients with MRI-conditional devices using strict safety protocols. Evidence has been building for safety in non-MRI conditional devices, but key patient groups, like the ones in PROMeNADe, have typically been excluded from studies.
Nevertheless, since 2011, the U.S. Centers for Medicare and Medicaid Services (CMS) has provided reimbursement coverage for non-MRI conditional MRI carried out through prospective registries. In their article, Gupta et al said that the PROMeNADE study is the largest in pacemaker-dependent patients with ICDs and the second largest in patients with abandoned leads.
The PROMeNADE study enrolled 532 patients with non-MRI conditional devices, including products manufactured by Medtronic, Abbott, and Boston Scientific. In total, the enrollees had 608 MRI clinically necessary studies, of which 61 were cardiac MRIs. Researchers excluded patients with ICDs implanted before 2000 or pacemakers implanted before 1998.
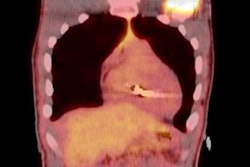
 Chest radiograph, posteroanterior view, in a 64-year-old woman with a history of heart transplantation demonstrates retained portion of right ventricular pacing lead and defibrillator lead with superior vena cava coil. The patient underwent five MRI examinations through a prospective registry study. Image courtesy of the Radiological Society of North America.
Chest radiograph, posteroanterior view, in a 64-year-old woman with a history of heart transplantation demonstrates retained portion of right ventricular pacing lead and defibrillator lead with superior vena cava coil. The patient underwent five MRI examinations through a prospective registry study. Image courtesy of the Radiological Society of North America.Precautions were taken during the imaging studies, including monitoring of patients for abnormalities and asynchronous pacing for the 27% of patients who were pacemaker-dependent. Studies were most commonly ordered for evaluation of the head and spine, followed by the hips/pelvis and shoulder or knee.
On the safety front, researchers had been looking out for device malfunctions such as a change in battery voltage and/or a reset of programmed parameters in devices. Potential clinical adverse events include arrhythmias, syncope, and death.
As it turned out, only one adverse event was reported, and it was related to device function (lead impedance change > 10%). Exclusion of pacemakers implanted before 1998 and ICDs implanted before 2000 may help explain the lack of device-related adverse events reported in the PROMeNADe study, according to the authors.
Safety is particularly of concern for MRI studies of organs that are closer to an implanted device. But, importantly, no adverse events were reported for 83 MRI studies of the thoracoabdominal region.
The study also documented benefits for patient management. Retrospective surveys of referring physicians showed that the MRI led to a change in diagnosis in 25% of cases, changed suspected prognosis for 26%, and altered planned medical or surgical treatment for 42%, the authors reported.