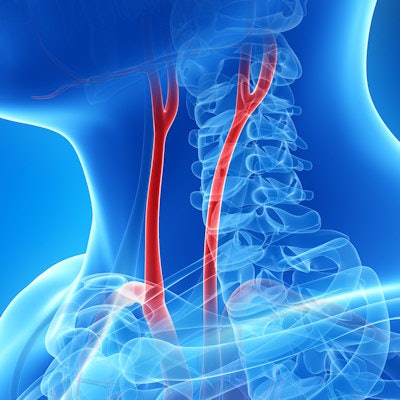
The U.S. Preventive Services Task Force (USPSTF) is advising against screening for asymptomatic carotid artery stenosis in the general adult population in a final recommendation statement published February 2 in JAMA.
The recommendation is consistent with the task force's 2014 statement, which graded carotid artery stenosis screening a D. The reason for the low grade is that the harms of carotid artery screening outweigh the benefits, according to USPSTF member Dr. Michael Barry of Massachusetts General Hospital in Boston.
"The Task Force wants to help prevent people from having a stroke, but screening for coronary artery stenosis is not an effective way to do so," he said in a USPSTF statement. "Unfortunately, screening for coronary artery stenosis in adults without symptoms does more harm than good, and we continue to recommend against it."
Carotid artery stenosis affects extracranial carotid arteries, and asymptomatic carotid artery stenosis refers to stenosis in persons without a history of ischemic stroke, transient ischemic attack, or other neurologic symptoms referable to the carotid arteries, the task force wrote in the JAMA article. Screening for the disease is accomplished through a variety of imaging modalities, including carotid duplex ultrasonography, MRI angiography, and CT angiography.
But these screening exams just aren't effective, according to the task force.
"The USPSTF found no externally validated risk stratification tools that could reliably distinguish between asymptomatic persons who have clinically important carotid artery stenosis and persons who do not, or the risk of stroke related to carotid artery stenosis," it wrote.
In an editorial also published in JAMA on February 2, Dr. Larry Goldstein, a neurologist at the University of Kentucky in Lexington, lauded the USPSTF's position.
"The estimated population-attributable risk for stroke related to asymptomatic carotid artery stenosis is approximately 0.7%, a risk considerably lower than for other stroke risk factors such as hypertension, atrial fibrillation, cigarette smoking, and hyperlipidemia," Goldstein wrote. "There remains no validated risk stratification tool for identifying a subpopulation of adults with a prevalence of asymptomatic carotid artery stenosis with a higher population-attributable risk that would lead to a benefit of intervention beyond risk factor management.'
Others pushed back, suggesting that the task force did not include evidence of the benefits of screening in its evaluation process -- or consideration of risk factors that occur in almost a third of U.S. adults, such as high blood pressure, hyperlipidemia, diabetes, smoking, limited physical activity, and poor diet.
"Without a true randomized clinical trial to directly answer the question, there is a lack of consensus and clarity on the role of carotid ultrasonographic screening for prevention of stroke in individuals who are asymptomatic," wrote Dr. Rebecca Smith-Bindman of the University of California, San Francisco in a JAMA Network Open editorial. "Nearly all of the specialty societies actually agree with the USPSTF and recommend against screening with carotid ultrasonography. However, these strong statements against screenings are all followed by the list of exceptions of individuals who, based on risk factors or characteristics, should in fact be screened."