MRI demonstrates superb performance in identifying breast lesions where surgical removal is required for women with suspicious nipple discharge, according to new research published April 13 in European Radiology.
The study authors, led by Dr. Martine Boisserie-Lacroix from Institute Bergonié in France, found that MRI has "excellent" sensitivity and negative predictive value for detecting a lesion requiring excision in patients who had otherwise normal mammograms and ultrasounds.
Nipple discharge has a reported prevalence of 3% to 10% in women undergoing routine imaging examinations. While an isolated milky or green nipple discharge is considered physiological, discharges that are orange and bloody, unilateral, spontaneous, and persistent may reveal underlying lesions. Malignant lesions can occur in 5% to 21% of cases, the researchers noted.
Mammography and ultrasound are the go-to imaging techniques, but they are limited in performance.
The current study covered 102 patients in a multicenter trial that took place between 2013 and 2019. In all, 48 patients had lesions requiring excision. By using MRI, the research team identified 46 of these.
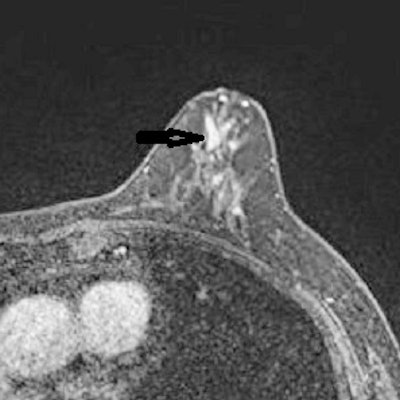
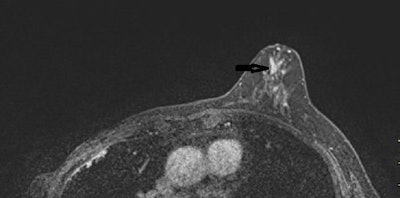 A 53-year-old woman with previous right mastectomy and uniporous left bloody discharge. Above: MRI axial plane after injection with fat saturation shows a left nonmass enhancement with linear distribution in the inner inferior quadrant (arrow). Below: Second-look ultrasound demonstrates three ducts of normal caliber in correlation (arrow). 10-G vacuum-assisted biopsy under ultrasound guidance revealed papilloma removed by surgical excision. Images courtesy of Dr. Martine Boisserie-Lacroix and European Radiology.
A 53-year-old woman with previous right mastectomy and uniporous left bloody discharge. Above: MRI axial plane after injection with fat saturation shows a left nonmass enhancement with linear distribution in the inner inferior quadrant (arrow). Below: Second-look ultrasound demonstrates three ducts of normal caliber in correlation (arrow). 10-G vacuum-assisted biopsy under ultrasound guidance revealed papilloma removed by surgical excision. Images courtesy of Dr. Martine Boisserie-Lacroix and European Radiology.
| Performance of MRI for detecting cases of nipple discharge requiring excision | |
| Sensitivity | 96% |
| Specificity | 85% |
| Positive predictive value | 85% |
| Negative predictive value | 96% |
Focusing on malignancy, MRI's negative predictive value and sensitivity were 100%.
Changes in patient management because of MRI follow-up could reduce morbidity and costs by avoiding unnecessary surgery, such as pyramidectomy, a pyramid-shaped tissue dissection often used in cases of suspicious nipple discharge.
"These results indicate that pyramidectomy may be unnecessary in MRI-negative patients where spontaneous resolution of nipple discharge was observed in most cases," the authors wrote.
The team also pointed out that unlike previously published studies which have been mostly retrospective, patients were enrolled consecutively in the prospective multicenter trial with homogeneous criteria.
Study limitations included digital breast tomosynthesis not being used at the beginning of the study. It also may be possible that a follow-up for more than one year or systematic surgical excision could have detected low-grade ductal carcinoma in situ (DCIS).
"But some of these low-grade DCIS are considered 'overdiagnosis' and a disadvantage of MRI when used in systematic screening," the authors wrote.



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











