Researchers from the universities of Oxford and Cambridge, U.K., have developed a protocol for proton MR spectroscopy (MRS) for evaluating brainstem function in patients recovering from COVID-19. They received a magna cum laude award at the International Society for Magnetic Resonance in Medicine (ISMRM) annual congress.
SARS-CoV-2 attacks the central nervous system, and a particularly nasty symptom is a feeling of breathlessness that can persist for months after acute infection has subsided, explained first author Carina Graf, a doctoral student at the Wolfson Brain Imaging Centre, University of Cambridge, and colleagues.
In their ISMRM poster, the group proved the feasibility of profiling brainstem neurochemistry in anticipation of a multisite clinical study across the U.K.'s 7-tesla MRI facilities.
"Based on early MRI observations in hospitalized patients, we hypothesized that COVID-19 may cause inflammation or degeneration of the brainstem where the respiratory control centers are located, leading to these symptoms," the authors noted.
Vast potential of MR spectroscopy
MR spectroscopy is a powerful method to probe the biochemistry of the central nervous system by measuring the concentrations of key neurometabolites, they stated.
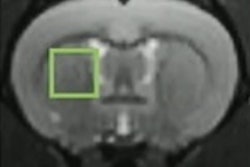
In the Oxbridge study, the main aim was to assess levels of myo-inositol (Ins, a marker of neuroinflammation), as well as the neurotransmitters gamma aminobutyric acid (GABA) and glutamate and markers of neurodegeneration such as creatine (Cr). The team knew these could be measured reproducibly in the cerebrum with single-voxel semi-LASER proton MRS at 7 tesla, but few previous studies had performed proton MRS assessments in the brainstem -- the region containing the respiratory control centers thought to be responsible for breathlessness in COVID-19 cases.
The researchers scanned the brainstem of patients who had recovered from COVID-19 (hospitalized and nonhospitalized). They used two 7-tesla MRI scanners (Magnetom 7T and Magnetom Terra, Siemens Healthineers). A total of 24 participants -- three to six months after a diagnosis of COVID-19 -- were recruited.
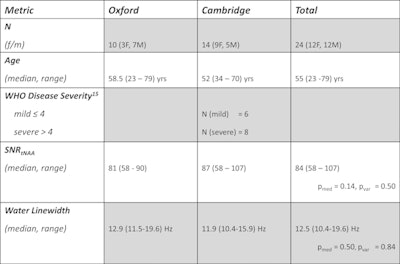 Patient population and spectral quality metrics. Uncorrected p-values for the Wilcoxon rank sum test (pmed) and Brown-Forsythe test (pvar) for equality of variances are reported. Reference 15 = World Health Organization (WHO), COVID-19 Therapeutic Trial Synopsis, 2020. Table and figure courtesy of Carina Graf and colleagues and ISMRM 2021.
Patient population and spectral quality metrics. Uncorrected p-values for the Wilcoxon rank sum test (pmed) and Brown-Forsythe test (pvar) for equality of variances are reported. Reference 15 = World Health Organization (WHO), COVID-19 Therapeutic Trial Synopsis, 2020. Table and figure courtesy of Carina Graf and colleagues and ISMRM 2021.Data were acquired at two sites (Wolfson Brain Imaging Centre and Wellcome Centre for Integrative Neuroimaging in Oxford) using scanners equipped with the same 1Tx/32Rx head coil (Nova Medical). Subjects were scanned with a one-hour protocol containing localizers, structural scan (0.7-mm3 isotropic MP2RAGE sequence matching UK7T Network protocols), proton MRS (using the CMRR semi-LASER MRS C2P package with a 12 x 12 x 20-mm3 voxel positioned at the pontomedullary junction), and quantitative susceptibility mapping and resting-state functional MRI contrasts.
For spectroscopy, the researchers followed the CMRR MRS C2P recommended procedure. The main acquisition used semi-LASER with 120 signal averages, 26-msec echo time, and 5,000-msec repetition time. Non-water suppressed spectra were acquired for water scaling and eddy-current correction. They used GOIA-WURST pulses for semi-LASER.
Spectra from both sites were preprocessed, analyzed, and quantified with Osprey. Metabolite concentrations were scaled relative to water and corrected for water relaxation losses. Nonparametric statistical analysis was performed in MATLAB R2019b with α = 0.05.
Spectral quality for both sites was high in all participants, with all but one spectrum exhibiting "acceptable" or better water linewidths of ≤ 19 Hz and a median signal-to-noise ratio for total N-acetylaspartate (NAA) of 84 (range, 58-107). Mean spectra averaged across all participants demonstrated the consistently high-quality spectra achievable at each site, and the consistency between sites.
Comparing sites statistically, there were no significant differences between the means and variances of signal-to-noise ratio for total NAA and water linewidths between the Oxford and Cambridge patients (p > 0.11), the authors reported.
Metabolite concentrations of Cr, GABA, glutamine, glutamate, Ins, NAA, and phosphocholine (normalized to tissue water) highlighted significant differences between metabolite concentrations at both sites for glutamine, Ins, and NAA (p[glutamine] = 0.024, p[Ins] = 0.021, p[NAA] = 0.018). However, no significant differences were found for the variances of all metabolites at both sites (p[Cr, GABA, glutamine, glutamate, Ins, NAA, phosphocholine] > 0.104).
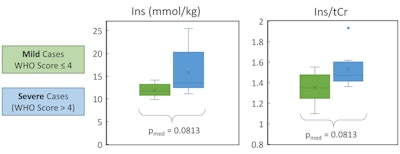 Impact of disease severity on metabolic marker of inflammation. Ins (water references) and Ins/tCr both showed a trend to increase with COVID disease severity. However, note that neither difference was statistically significant for the study cohort. This observation is biologically plausible since Ins reflects neuroinflammation, but it needs to be tested in a larger cohort and/or against matched controls to understand whether it is a real effect or not.
Impact of disease severity on metabolic marker of inflammation. Ins (water references) and Ins/tCr both showed a trend to increase with COVID disease severity. However, note that neither difference was statistically significant for the study cohort. This observation is biologically plausible since Ins reflects neuroinflammation, but it needs to be tested in a larger cohort and/or against matched controls to understand whether it is a real effect or not.A preliminary investigation of Ins showed a trend for increasing Ins with COVID-19 disease severity, but this did not reach statistical significance in the small cohort for Ins (water referenced) or Ins/total creatine (tCr) (p[Ins] = 0.081, p[Ins/tCr] = 0.081) between cases of mild and severe COVID-19, the authors wrote.
"The small differences in metabolite concentrations may be explained by differences in the patient cohorts between the sites," they explained. "The possible trending increase in Ins or Ins/tCr with severe vs mild COVID-19 would be consistent with neuroinflammation in the brainstem, although we emphasize that this is not yet a statistically significant finding from our small cohort."
Evolution of 7T MRI in U.K.
Cambridge's 7-tesla MRI scanner was installed in 2016, funded by a Medical Research Council (MRC) infrastructure investment. The MRC encouraged all U.K. sites with 7-tesla MRI scanners to join forces in establishing the UK7T Network. Dr. Chris Rodgers, head of 7-tesla MRI physics in Cambridge, previously worked for 13 years in Oxford, and continues to hold a visiting academic appointment there.
"Given these strong links, when COVID struck, we were keen to think how 7T MRI could contribute," Graf told AuntMinnieEurope.com. "These conversations began separately at our two centers. But it soon became clear that we could both benefit from joining forces to adapt the UK7T protocols to do spectroscopy and complementary imaging in the brainstem. This led to the ISMRM 2021 abstract and to ongoing joint grant applications."
The Oxbridge group is now recruiting a set of age- and sex-matched healthy controls at the two sites. They hope soon to be able to confirm whether there are alterations in neurochemistry in patients recovering from COVID-19. They have recently submitted a funding bid to perform a larger-scale investigation of brainstem effects in COVID-19 across the U.K.'s 7-tesla MRI sites.
According to Graf, "Studies involving patient populations at multiple 7T sites are still rare, due to a lack of standardization and availability of hardware. However, with the number of 7T sites increasing rapidly, we believe it is imperative to demonstrate that joint efforts provide immense benefits for conducting large-scale studies at 7T, for instance by reaching a larger percentage of the population."
The group has received funding to continue pilot studies from the Addenbrooke's Charitable Trust and from the National Institute for Health Research (NIHR) Cambridge Biomedical Research Centre to continue the 7-tesla MRI project and other closely related studies using 3-tesla MRI to better understand COVID-19. It has just applied to the NIHR for substantive funding in a bid led by Kyle Pattinson, consultant anesthetist and associate professor at Oxford, with Cambridge, Nottingham, and Cardiff as partners.
"In the future, we are keen to investigate the specificity of metabolic changes and their correlation with clinical outcomes in order to establish MR spectroscopy as a noninvasive biomarker to monitor patients recovering from COVID-19," Graf commented.