Up to 40% of COVID-19 survivors experience long-term neurological conditions, and it's crucial that radiologists understand these, according to a May 17 presentation at the International Society for Magnetic Resonance in Medicine (ISMRM) 2021 virtual annual meeting.
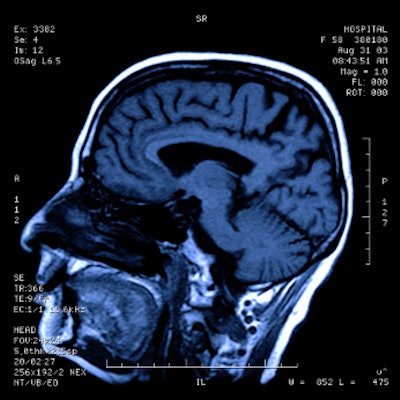
The good news is that MRI has shown itself to be an effective way to track COVID-19's lasting neurological effects, according to presenter Dr. Simonetta Gerevini of Azienda Ospedaliera Papa Giovanni XXIII hospital in Bergamo, Italy.
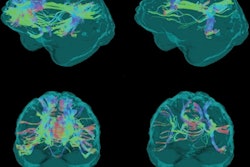
"Neuroimaging can illuminate a spectrum of central nervous system abnormalities, from ischemic lesions and microhemorrhages to meningoencephalitis and white matter lesions," she noted.
Long-term neurological and neuropsychological sequelae are reported in up to 30% to 40% of COVID-19 survivors. Symptoms can include fatigue, myalgia, headache, dysautonomia, and cognitive impairment, according to Gerevini.
"There's growing evidence of neurological manifestations in patients with COVID-19," she told ISMRM session attendees. "Correct estimation of incidence and prevalence is difficult because ... of a lack of data, [but we see these more frequently] in patients with comorbidities ... and those with multiple organ dysfunction."
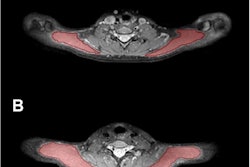
In her talk, Gerevini reviewed the hypothesis of how the SARS-CoV-2 virus invades the nervous system through the blood-brain barrier or via peripheral nerves. She listed the most commonly reported MRI findings in patients with severe COVID-19 who are on ventilation and in the intensive care unit:
- Leukoencephalopathy, microhemorrhages, and acute/subacute infarcts
- White-matter injury and large, parenchymal hemorrhages
- Acute infarctions and leptomeningeal enhancement
- Posterior reversible encephalopathy syndrome (PRES) and hemorrhagic infarction
- Acute disseminated encephalomyelitis (ADEM)-like white matter lesions and microhemorrhages
Gerevini cited studies that showed an 0.8% to 6% chance of stroke in hospitalized patients with COVID-19, a risk that increases with the severity of the infection. She also cited a study that found concerning rates of various types of thromboembolism in COVID-19 patients, including large infarctions (44.5%), lacunar infarctions (24%), and hemorrhagic stroke (24%).
"Neurological outcomes are variable depending on comorbidities, but stroke and hemorrhage are reported widely and not uncommonly in younger patients, and [subacute and chronic] patients, particularly those on ventilators in the intensive care unit, [can develop] leukoencephalopathy and microhemorrhages," she said.
Yet despite these concerning neurological long-term effects of COVID-19, brain MRI -- particularly advanced techniques such as diffusion-weighted, diffusion-tensor, and functional MRI -- has been shown to be an effective way to track these effects, according to Gerevini.
"Brain MRI is very useful to image the complications of SARS-CoV-2 infection in the brain in acute, subacute, and chronic phases," she concluded.