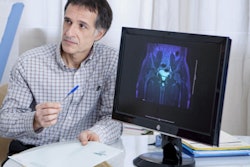
Multiparametric MRI (mpMRI) is an effective screening tool for prostate cancer, but not all eligible patients are receiving it -- especially Black men, who tend to have higher rates of the disease, according to a study published May 19 in Academic Radiology.
The study results demonstrate a continued need to explore, understand, and mitigate healthcare disparities, particularly around cutting-edge screening technology, wrote a team led by Christiane El Khoury of Stony Brook University in New York City.
"Our findings illustrate the importance of disparity awareness in prostate cancer mpMRI and highlight the need to examine additional mpMRI disparities across other races and social determinants," the group wrote.
Black American men are 1.7 times more likely to have prostate cancer than their white counterparts, and their mortality rate is twice as high, El Khoury and colleagues noted. Multiparametric MRI is the most advanced -- yet most expensive -- diagnostic test for prostate cancer, and it may not be equally available to all eligible men.
El Khoury's team sought to explore potential disparities in the use of mpMRI through a literature review that included 17 studies published between 2014 and 2017 that investigated disparities in the use of the technology as well as its performance among Black men. Of these 17 studies, five were population-based, 10 were from single institutions, and two were multi-institutional.
The researchers found inequity in mpMRI use across race, age, income, time of diagnosis, region, and insurance status, with lower utilization among Black, poor, and uninsured men. One study found that Black men had an odds ratio of 0.64 for being less likely to undergo mpMRI compared with white men.
"The most common predictor for mpMRI utilization was race," the team noted. "In fact, all analyses agreed that African Americans were less likely to undergo mpMRI versus non-African Americans."
The team also found, however, that mpMRI performed either comparably or better in Black men compared with their white counterparts, finding regions of interest in 24% of Black men compared to 12% in non-Black men. Black men who had previously received a negative transrectal ultrasound biopsy were more likely to have suspicious anterior prostate lesions on mpMRI compared with their white peers (odds ratio, 1.81), and twice as likely to have tumors that were upgraded to more serious disease.
Multiparametric MRI must be made available to populations who can benefit from it -- and physician education would help, according to El Khoury and colleagues.
"Future research should address physician interaction and evaluate whether all imaging options are discussed," they wrote. "Ideally, both the referring physician and the radiologist should share the task to completely inform their patients about imaging options in a way that is unbiased by patient's age, socioeconomic status, and procedure cost. Therefore, emphasizing health disparities education for physicians is an important step in reducing unfair distribution of care."