
Do messenger RNA (mRNA) COVID-19 vaccines cause myocarditis? Perhaps -- but not on a scale that should prevent people from getting vaccinated, according to two studies published June 29 in JAMA Cardiology.
In the first study, out of seven patients who underwent cardiac MRI and were diagnosed with myocarditis, four individuals had recently received an mRNA COVID-19 vaccine. However, this was in the context of more than 550,000 people who had been fully vaccinated without complications.
In the second study, researchers identified 23 military patients who developed myocarditis after receiving an mRNA COVID-19 vaccine -- but again, this was out of 2.8 million doses administered during the study period.
Vaccine-associated myocarditis has mostly been described anecdotally, and a causal relationship between COVID-19 vaccines and the heart condition is difficult to establish, noted a team led by Dr. Han Kim of the Duke Cardiovascular Magnetic Resonance Center in Durham, NC. He and his colleagues sought to investigate the occurrence of COVID-19 vaccine-related myocarditis between February and April of this year.
The group's study cohort consisted of seven individuals diagnosed with acute myocarditis on cardiovascular MRI between February and April of 2021. Of the seven, four developed the condition within five days of receiving an mRNA COVID-19 vaccine; all four had received a second dose (two had Moderna and two had Pfizer).
The four included three men between the ages of 23 and 36 and a 70-year-old woman, and all of whom presented to the hospital with severe chest pain and biomarker evidence of myocardial injury. Their cardiac MRI findings were typical for myocarditis; all were hospitalized, underwent treatment for the condition, and were released within two to four days.
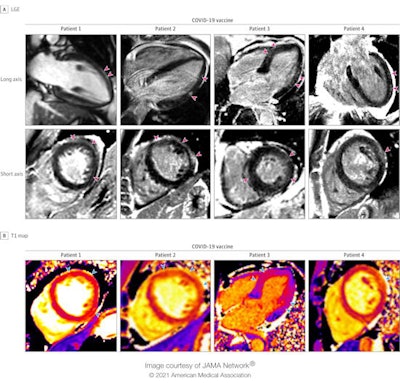 Cardiac MRI scans of patients with acute myocarditis following COVID-19 vaccination. Late gadolinium enhancement (LGE) images and T1 maps are shown in four patients who recently received a COVID-19 vaccine. Patients 1, 2, and 4 demonstrate epicardial LGE, and patient 3 demonstrates patchy, diffuse LGE (pink arrowheads), which are consistent with myocarditis. T1 maps demonstrate abnormal (elevated) native T1 in the regions with late gadolinium enhancement (blue arrowheads). Image and caption courtesy of JAMA Cardiology.
Cardiac MRI scans of patients with acute myocarditis following COVID-19 vaccination. Late gadolinium enhancement (LGE) images and T1 maps are shown in four patients who recently received a COVID-19 vaccine. Patients 1, 2, and 4 demonstrate epicardial LGE, and patient 3 demonstrates patchy, diffuse LGE (pink arrowheads), which are consistent with myocarditis. T1 maps demonstrate abnormal (elevated) native T1 in the regions with late gadolinium enhancement (blue arrowheads). Image and caption courtesy of JAMA Cardiology.Although a causal relationship between the COVID-19 vaccine and acute myocarditis in these patients can't be definitively established, there appeared to be no other obvious reason for the injury, Kim and colleagues noted.
"[None of these patients] had a viral prodrome or had coincident testing (including COVID-19 polymerase chain reaction and respiratory virus polymerase chain reaction) that revealed an alternative explanation," they wrote. "None had COVID-19 in the prior year, suggesting that myocarditis from subsequent multisystem inflammatory syndrome is also unlikely."
The second study was led by Dr. Jay Montgomery of Walter Reed National Military Medical Center in Bethesda, MD, and included 23 military men (22 currently serving and one retiree), all of whom received an mRNA COVID-19 vaccine and developed myocarditis symptoms following the second dose. All of the patients recovered.
The results of the two studies suggest that developing myocarditis after receiving an mRNA-based COVID-19 vaccine is rare, according to an accompanying editorial penned by a team led by Dr. David Shay of the U.S. Centers for Disease Control and Prevention's COVID-19 Response Team in Atlanta.
"Kim et al estimated that more than 560,000 persons in the six counties surrounding their tertiary care institution had received two doses of an mRNA-based COVID-19 vaccine by April 30, 2021; they detected four myocarditis cases by that date," Shay and colleagues wrote. "The Military Health System administered more than 2.8 million doses of mRNA-based vaccines through April 30, 2021, and detected 23 myocarditis cases. ... Based on currently available data, myocarditis following immunization with current mRNA-based vaccines is rare."
But results of the study could further spook people who are already leery of getting vaccinated, noted a team led by Dr. Ann Marie Navar, PhD, of the University of Texas Southwestern Medical Center in Dallas, in another editorial.
"Prior reports of adverse events following immunization for measles, mumps, and rubella, later deemed unsubstantiated, raised significant public alarm and led to vaccine resistance -- an effect that lingers to this day," the group wrote. "In light of this legacy, as well as ongoing fears related to vaccination leading to variable uptake, especially in populations at higher risk for COVID-19, the editorial decision [to publish this study] was not taken lightly."
Clinicians need to be in conversation with patients, Navar's team concluded.
"In addition to discussing the risks of COVID-19 infection and the efficacy of vaccines, physicians should identify patient concerns regarding vaccine safety and be prepared to discuss these risks with patients," Navar and colleagues wrote.





















