MRI-guided focused ultrasound can be superior to external-beam radiation therapy when it comes to pain relief and quality of life for metastatic bone disease patients, according to research presented November 30 at the RSNA 2021 annual meeting.
Dr. Giulia Alfieri from the University of Rome in Italy presented results from a study her team led that showed that this ultrasound application can help in patients with metastatic pain in the pelvis, sternum, long bones, and ribs.
"MRI-guided focused ultrasound should be considered as a palliative alternative to external-beam radiation therapy in patients with painful bone metastases in specific anatomical sites," Alfieri said.
Bone metastases affect about 280,000 people in the U.S. and are the most common cause for cancer-related pain. They can also affect multiple areas of an individual's quality of life.
Standard external-beam radiation therapy is the standard of care for bone metastases. However, researchers have touted MRI-guided focused ultrasound as being noninvasive and emitting no radiation, as well as being able to precisely target metastases and provide real-time temperature monitoring.
Alfieri et al wanted to assess the efficacy and safety of this newer method and compare it with standard external-beam radiation therapy for the palliative treatment of painful bone metastases.
The team looked at 198 patients from two centers, all of whom were over 18 years old. Patients included in the phase II trial were diagnosed with cancer and pain corresponding to radiologically confirmed bone metastases. Their pain was measured as greater than a score of 4 on a visual analogue scale. The researchers also did follow-up of one, two, three, six, and 12 months with the patients.
Out of the 198 patients, 100 were assigned to the MRI-guided focused ultrasound group, while the other 98 were assigned to the external-beam radiation therapy group.
The study authors found that 91 patients in the ultrasound group showed either complete or partial response to this treatment method, compared with 66 in the radiation therapy group (p < 0.001).
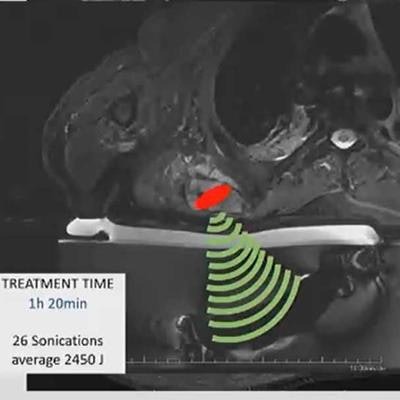
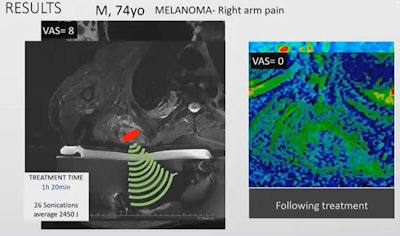 MRI-guided focused ultrasound can be an alternative method for palliative treatment of cancer patients with bone metastases, researchers said. Here, a 74-year-old male patient with arm pain related to melanoma received such treatment and reported a visual analogue scale score of 0 for pain. Before treatment, the score was 8, indicating severe pain. Image courtesy of Dr. Giulia Alfieri.
MRI-guided focused ultrasound can be an alternative method for palliative treatment of cancer patients with bone metastases, researchers said. Here, a 74-year-old male patient with arm pain related to melanoma received such treatment and reported a visual analogue scale score of 0 for pain. Before treatment, the score was 8, indicating severe pain. Image courtesy of Dr. Giulia Alfieri.One patient Alfieri highlighted was a 74-year-old male patient who exhibited right arm pain after being diagnosed with melanoma, with a visual analogue score of 8. The patient underwent MRI-guided focused ultrasound treatment for one hour and 20 minutes with 26 sonications. After treatment, the patient had a visual analogue score of 0.
Quality-of-life questionnaires showed no significant difference between the two groups. However, analysis of a questionnaire for palliative care showed significant data for areas of physical function, appetite, nausea and vomiting, dyspnea, and quality of life in favor of MRI-guided focused ultrasound.
Meanwhile, adverse effects were seen in 15% of the ultrasound group and 24% of the radiation therapy group.
Alfieri noted that larger, randomized clinical trials are needed to validate these results. She also said that MRI-guided focused ultrasound still faces barriers compared to standard radiation therapy.
"The limitations are that MRI-guided focused ultrasound is less available, it takes more time in comparison to external-beam radiation therapy ... and to date, the costs for ultrasound treatment are higher in comparison with external-beam radiation therapy," Alfieri said.





















