LONDON - Take great care when it comes to the quench button, a specialist on MRI safety standards warned on Saturday at the annual meeting of the International Society for Magnetic Resonance in Medicine (ISMRM).
"Sadly, one Indian site disabled it, with ultimately severe consequences," said Michael Steckner, PhD, a medical physicist who has been a member of the ISMRM Safety Committee since 2013. "Enhanced requirements to check the quench system are always operative, and the button still works in cases of power loss and redundancy and automatically self-checks for functionality."
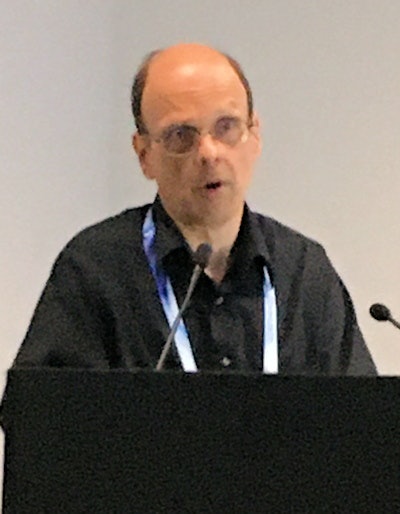 Michael Steckner, a longstanding member of the ISMRM Safety Committee.
Michael Steckner, a longstanding member of the ISMRM Safety Committee.ISMRM is holding this week's meeting in conjunction with the European Society for Magnetic Resonance in Medicine and Biology and the International Society for MR Radiographers and Technologists.
What's driving MRI safety
The main drive in MRI safety right now is to improve the consistency of defined terms, provide greater transparency and accessibility to essential information, and boost control of scanner outputs to simplify implant scanning, he noted at a well-attended session on the opening day of ISMRM 2022.
Acoustic noise is another important area, and it's vital to get the basics right, such as helping patients to properly apply hearing protection, following vendors' recommendations, and using properly labeled, unmodified methods, continued Steckner, who is senior manager of MR research at Canon Medical Research USA, Beachwood, Ohio, U.S.
"MR vendors provide recommended hearing protection based on maximum patient exposure measurements," he said. "They independently apply risk management."
Within the European Union, directives require vendors to supply exposure values for an average worker, but this is difficult for MRI and is a test method in development.
New safety standards in these areas are expected to be published in late 2022, but regulators typically give a two- to three-year window before a standard becomes the "expected" implementation, Steckner pointed out. "Using B1+rms (the "root mean square" value of B1+ averaged over a period of 10 seconds) rollout as an example, MR vendors 'guesstimate' that 50% of the installed base had it after five years."
Importance of terminology, labeling, and training
Single terminology, clear labeling, and more information are central to MRI being conducted more safely around the world, Ilse Patterson, lead R&D MRI radiographer at Cambridge University Hospitals, U.K., told ISMRM attendees at the same session.
Make sure your hospital's information and "about" function are easily accessible, especially in multisystem departments with different vendors' technology and scanners operating at different field strengths, she said.
MR output conditioning (MROC) looks set to change how implant scanning is conducted, but imaging of some patients with implants will still have to rely on specialist nurses, physiologists, clinicians, or vendor representatives to adapt the pre- and post-MRI setting.
"Some hospitals do not have this clinical support," Patterson said. "It's possible that radiographers are more familiar with specific absorption rate (SAR) and slightly less familiar with B1+rms."
Overall, there is still a need for local policies to reflect the recommendations that are left "up to us," she remarked.
"New planning and design guidelines are very helpful," she said. She welcomes the current moves toward better acoustic noise information and spatial field strength changes, but she also said that MRI safety training remains the single most important aspect.
 This patient suffered a thermal burn due to delayed MR heating after a 1.5-tesla scan. The U.K. Medicines and Healthcare products Regulatory Agency (MHRA) were told about the incident, and the vendor changed the coil that caused the injury. Image courtesy of Ilse Patterson.
This patient suffered a thermal burn due to delayed MR heating after a 1.5-tesla scan. The U.K. Medicines and Healthcare products Regulatory Agency (MHRA) were told about the incident, and the vendor changed the coil that caused the injury. Image courtesy of Ilse Patterson.There is no hard stop for specific absorption limits anymore, and this development is particularly important for interventional systems, she added.
Scanning implants
Some hospitals are reluctant to scan patients with implants because of a lack of experience/confidence, absence of medical physics support, limited ability to control the gradient slew rate/rise-time, and misleading labeling from implant vendors. Also, it can be challenging to manually configure low SAR sequences, Patterson explained.
She listed the following ideal requirements for implant scanning:
- Understand MRI safety requirements for implants.
- Make the technology accessible to every patient that has MRI-conditional implant(s).
- Improve service for patients with implants.
- All MRI scanners must adapt to implant imaging conditions.
- Develop an ability to have clear implant labeling and uniform technology.
- Confirm whether MRI units scan patients with implants without additional physics support.