Few women with silicone breast implants comply with the U.S. Food and Drug Administration's (FDA) recommendation that they be tracked for asymptomatic rupture with breast MRI, a study published June 3 in Plastic and Reconstructive Surgery has found.
Why? It may be that women with silicone implants don't know about the FDA guideline, or they may not see it as necessary, reported a team led by Dr. Libby Copeland-Halperin of Dartmouth-Hitchcock Medical Center in Lebanon, NH.
"[The] majority of patients in our study were unaware of [the FDA recommendation] and generally underwent imaging for cancer-related reasons rather than implant concerns," the group wrote. "Furthermore, those who were aware of the recommendation elected not to undergo screening due to having no implant concerns or aversion to MRI testing."
Silicone breast implants were introduced in the 1960s. Rupture is one of the most common reasons for removing them -- with some estimates putting rupture incidence as high as 30% at five years, 50% at 10 years, and 70% at 17 years. Silicone leakage is a serious concern because it can have systemic effects, Copeland-Halperin and colleagues noted.
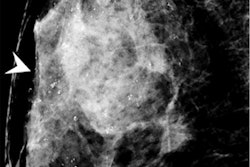
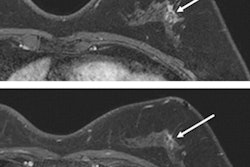
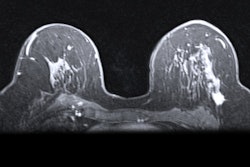
Mammography can identify ruptures in which silicone has migrated out of the implant (extracapsular), but it may miss those in which the silicone has ruptured in a capsule of tissue the body has formed around the implant (intracapsular), the authors wrote. Additionally, although breast implant ruptures may manifest as breast asymmetry or pain, they can also be asymptomatic, which makes breast MRI a more effective way to assess for implant ruptures. In 2006, the FDA recommended that women with silicone implants undergo breast MRI beginning three years postsurgery and every two years after that.
But are women complying with this guideline? To address this question, the investigators conducted a telephone survey study that included 109 women 18 years and older with silicone implants that had been placed between 2011 and 2016. The survey assessed the women's awareness of FDA recommendations, whether they had undergone breast MRI for screening for asymptomatic implant rupture, and if there were any barriers to doing so. Most of the women (79%) had implants placed for reconstruction purposes, and most (30%) were covered by Medicare or Medicaid.
Yet, of the women who participated in the survey, only 5.9% were aware of and compliant with the FDA's breast MRI follow-up recommendation; 92 were "unaware of the FDA recommendation, despite this having been discussed during perioperative clinic visits and summarized in supplemental information pamphlets," the group reported.
| Rates of imaging surveillance for silicone implants | |
| Measure | Compliance rate |
| Any other imaging performed since implant surgery | 48.6% |
| Mammography performed since implant surgery | 31.2% |
| Ultrasound performed since implant surgery | 17.4% |
| MRI performed at all since implants placed | 15.6% |
| MRI performed within FDA guideline | 5.9% |
The researchers found no statistically significant difference in women's adherence when it came to cosmetic versus reconstructive surgery, having health insurance, or having higher income.
Lack of compliance with the FDA's suggestion regarding tracking silicone breast implant rupture with breast MRI may have to do with patient discomfort about the exam or insurance coverage, the team noted.
"Even patients who were aware of the recommendation elected not to undergo screening MRI because they 'didn't like MRIs' or did not believe it necessary because 'everything has been fine' in follow-up," Copeland-Halperin and colleagues wrote. "Unfortunately, because routine, asymptomatic follow-up visits several years postoperatively may not be covered by insurance policies and cosmetic procedures/follow-up are not covered by insurance, many patients may not return for follow-up around the time MRI would be due."
The low adherence rate needs further study in order to better understand women's reluctance, according to the authors.
"Additional research is needed to better characterize adherence to MRI surveillance recommendations, identify barriers to implementation, and determine whether [the FDA's] recommendation remains valid," they concluded.