Preoperative diffusion-weighted MRI (DWI-MRI) is effective for predicting whether biopsy-confirmed ductal carcinoma in situ (DCIS) will be reclassified as invasive cancer after surgery, a study published July 5 in Radiology has found.
The technique could translate into better surgical and treatment staging for women with DCIS, wrote a team led by Dr. Shin Ae Lee of Seoul National University College of Medicine in South Korea.
"DWI is an MRI technique that has been widely explored to differentiate benign from malignant breast lesions and can reduce the false-positive findings at conventional [dynamic contrast-enhanced] MRI," the group noted. "Therefore, DWI is increasingly incorporated into routine breast MRI protocols."
DCIS is usually diagnosed with percutaneous needle biopsy. Yet biopsy has limitations, and more than half of women (59%) diagnosed with DCIS are later reclassified to invasive cancer after surgery, and invasive cancer requires more detailed treatment planning, the group noted. Some surgeons go ahead and perform axillary staging during initial surgery for DCIS to avoid secondary procedures, but this may result in unnecessary intervention.
Breast MRI is used to preoperatively evaluate women with DCIS, particularly dynamic contrast-enhanced (DCE) MRI, but it can produce inconsistent results, and researchers have explored whether diffusion-weighted MRI might be more effective. As surgical staging models for DWI-MRI are scarce, Lee's group sought to develop and validate one that could help predict breast cancer reclassification in women with DCIS and to determine which women might benefit from sentinel node biopsy during initial surgery.
The study included 245 women who underwent both preoperative DCE and DWI-MRI scans between June 2019 and March 2020. The investigators used pathology results to confirm the presence of invasive cancer and any axillary metastases.
Of the total study cohort, 140 women were in the model development set and 105 in the validation set. Of these two groups, 41% (57 of 140) and 41% (43 of 105) had cancers that were reclassified as invasive after surgery.
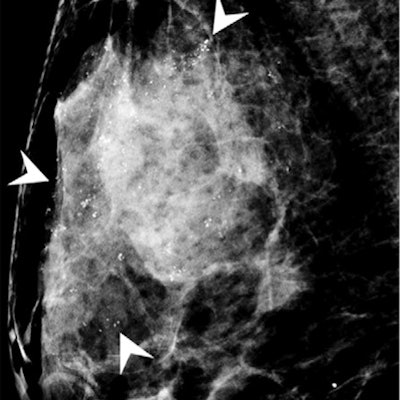
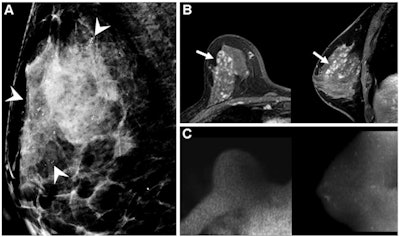 Images of a 46-year-old asymptomatic woman diagnosed with intermediate-grade ductal carcinoma in situ (DCIS) by 14-gauge needle biopsy. (A) Ultrasound image shows an irregular hypoechoic mass (arrow). Mammograms (not shown) showed heterogeneously dense breasts and did not show the lesion. (B) On preoperative contrast-enhanced axial (left) and sagittal (right) MRI scans, a 0.9-cm irregular enhanced mass was observed in the right lower inner breast (arrows). (C) Image from axial diffusion-weighted imaging (DWI) with b value of 1,200 sec/mm2 (left) and sagittal maximum intensity projection image (right) show high signal intensity (arrows) in the area corresponding to the enhanced lesion. Apparent diffusion coefficient (ADC) values were measured on the (D) fusion image of DWI and the ADC maps. Axial (left) and sagittal (right) fusion images were cross-referenced to ensure that the region of interest (ROI) was inside the tumor border and did not include the surrounding parenchyma. Images and caption courtesy of the RSNA.
Images of a 46-year-old asymptomatic woman diagnosed with intermediate-grade ductal carcinoma in situ (DCIS) by 14-gauge needle biopsy. (A) Ultrasound image shows an irregular hypoechoic mass (arrow). Mammograms (not shown) showed heterogeneously dense breasts and did not show the lesion. (B) On preoperative contrast-enhanced axial (left) and sagittal (right) MRI scans, a 0.9-cm irregular enhanced mass was observed in the right lower inner breast (arrows). (C) Image from axial diffusion-weighted imaging (DWI) with b value of 1,200 sec/mm2 (left) and sagittal maximum intensity projection image (right) show high signal intensity (arrows) in the area corresponding to the enhanced lesion. Apparent diffusion coefficient (ADC) values were measured on the (D) fusion image of DWI and the ADC maps. Axial (left) and sagittal (right) fusion images were cross-referenced to ensure that the region of interest (ROI) was inside the tumor border and did not include the surrounding parenchyma. Images and caption courtesy of the RSNA.The researchers found that a combination of DWI findings and clinical-pathologic factors (i.e., high breast tissue density, calcifications, lesion features [i.e., masses], and size of ≤ 5 cm) were linked to a higher risk of upstaging to invasive cancer after surgery, with an area under the receiver operating curve of 0.87 in the development group and 0.76 in the validation group. They also discovered that the rate of axillary lymph node metastasis was 4%, suggesting that "routine axillary staging at initial surgery in women with biopsy-proven DCIS is not justified."
The model's efficacy could help clinicians better tailor treatment and care for women with breast cancer, according to the authors.
"The predicted probability of invasive cancer by [our model] was a reproducible parameter for selecting women indicated for sentinel node biopsy at initial surgery, thus avoiding unnecessary axillary surgery and preventing delayed secondary surgery," they concluded.