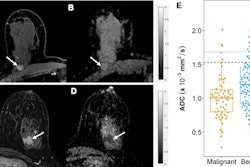
Restriction spectrum imaging (RSI) is a suitable method for evaluating neoadjuvant therapy response early for breast cancer, suggest findings presented December 6 at the San Antonio Breast Cancer Symposium.
In her presentation, Maren Andreassen, MD, PhD, from the University of California, San Diego discussed her team’s work, which found that a novel RSI cancer tissue classifier predicted response to neoadjuvant therapy after three weeks. The team also found that RSI could identify most cases with residual tumor at surgery.
“RSI performance was similar to performance by standard MRI by manual tumor measurement on dynamic contrast enhancement [DCE-MRI],” Andreassen said.
DCE-MRI is used to assess neoadjuvant therapy response for breast cancer treatment. However, Andreassen pointed out that this method needs expert radiologist readers to evaluate the change in longest tumor dimension during therapy, as well as administering gadolinium-based contrast agents.
Diffusion-weighted MRI (DWI) does not require contrast agents and detects the microscopic diffusion of water molecules. However, the commonly used DWI method, apparent diffusion coefficient, currently does not have full utility in breast imaging, Andreassen said.
She and colleagues evaluated the performance of RSI, a more recent DWI method, in automatically monitoring breast tumor size during neoadjuvant therapy. RSI allows for differentiating of restricted diffusion from cancer cells to that of normal tissue cells and extracellular water.
For the study, the team included 27 women who underwent 3T MRI at four time points during therapy. Of the total, 17 women received all four MRI scans. The women also had biopsy-proven unilateral invasive breast cancer 2.5 cm or larger with indication for neoadjuvant therapy.
 Maren Andreassen, MD, PhD, discussed her team's findings, which suggest that restriction spectrum imaging is a suitable alternative to assessing early response to neoadjuvant chemotherapy in breast cancer patients undergoing treatment. Image courtesy of Maren Andreassen.
Maren Andreassen, MD, PhD, discussed her team's findings, which suggest that restriction spectrum imaging is a suitable alternative to assessing early response to neoadjuvant chemotherapy in breast cancer patients undergoing treatment. Image courtesy of Maren Andreassen.
Also, tumor size as examined by RSI was assessed against manual DCE tumor size and average apparent diffusion coefficient values. Ten women in the study experienced pathologic complete response.
The team found that RSI was on par with DCE-MRI when predicting non-response at the early therapy time point of three weeks, represented by area under the curve (AUC) values. RSI also had better predictability than that of apparent diffusion coefficient. However, DCE-MRI outperformed RSI at later therapy time points.
| Comparison between MRI methods for predicting chemotherapy response (in AUC, with 1 as reference) | |||
|---|---|---|---|
| Therapy time points | Apparent diffusion coefficient | DCE-MRI | RSI |
| 3 weeks | 0.45 | 0.64 | 0.65 |
| 12 weeks | 0.35 | 0.71 | 0.6 |
| Post therapy | 0.36 | 0.8 | 0.76 |
Still, Andreassen highlighted that the RSI classifier is automatic while standard-of-care MRI by using DCE and apparent diffusion coefficient requires manual user input. This included an image acquisition time of four minutes, 25 seconds for RSI.
“This suggests that RSI may aid to cost-efficiently evaluate neoadjuvant therapy of breast cancer, with the aim to help guide clinical decision-making and enable tailored therapy regimens,” she said.
Andreassen also suggested that RSI could be a suitable alternative to DCE-MRI for patients who have adverse reactions toward contrast agents.
“RSI has a large potential to guide clinical decision-making and enable tailored therapy regimens, but large-scale validation studies in routine breast cancer follow-up are warranted,” she added.