Applying point-of-care apparent diffusion coefficient (ADC) cutoffs from diffusion-weighted imaging (DWI) could reduce MRI-prompted breast biopsies, a study published February 13 in Radiology found.
Researchers led by Inyoung Youn, MD, PhD, from the University of Washington in Seattle found that applying these cutoffs led to a nearly 16% decrease in breast biopsies. They also reported a tradeoff of lowered sensitivity for in situ and microinvasive disease manifesting as nonmass enhancements.
“Our study results support adoption of [ADC] cutoffs in the clinical setting, with the caveat that radiologists may need to be more cautious about using ADCs to avert biopsy of non-mass enhancement lesions,” Youn and co-authors wrote.
DWI is an MRI technique that uses no contrast, with previous research suggesting it can improve diagnostic accuracy in breast cancer detection. It reflects the diffusion of water molecules in tissue, which allows for lesions to be characterized at the micro level. Such measures can be quantified by ADCs.
The researchers highlighted that DWI takes “only a few minutes,” is available on various scanner platforms, and can be integrated into conventional breast MRI protocols.
The multicenter A6702 trial, led by the Eastern Cooperative Oncology Group–American College of Radiology Imaging Network Cancer Research Group, identified an optimal ADC cutoff to potentially reduce biopsies by 21% without affecting sensitivity. However, Youn and colleagues noted that it hasn’t been established whether this performance can be achieved in clinical settings.
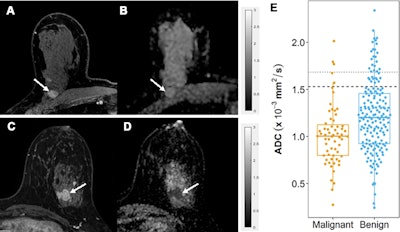 Apparent diffusion coefficient (ADC) measurements for benign and malignant BI-RADS category 4 or 5 lesions at MRI. (A, B) Benign BI-RADS category 4 lesion in a 55-year-old woman. (A) Dynamic contrast-enhanced MRI (DCE-MRI) scan shows a 12-mm, oval, circumscribed, homogeneous mass in the right posterior breast (arrow). (B) On the diffusion-weighted image, the lesion shows high diffusivity (arrow), with an ADC of 2.04 × 10-3 mm2/sec. Biopsy revealed benign fibroadenoma. (C, D) Malignant BI-RADS category 4 lesion in a 41-year-old woman. (C) DCE-MRI scan shows a 24-mm irregular, heterogeneous mass at the 3 o’clock position in the left breast (arrow). (D) On the diffusion-weighted image, the lesion demonstrates low diffusivity (arrow), with an ADC of 0.91 × 10-3 mm2/sec. Biopsy revealed invasive ductal carcinoma. All MRI scans are shown in the axial plane. (E) Box plot shows ADC measurements for 240 BI-RADS 4 and 5 lesions (63 malignant and 177 benign). Both prespecified optimal and conservative ADC cutoffs are indicated on the plot for reference: 1.53 × 10-3 mm2/sec (dashed line) and 1.68 × 10-3 mm2/sec (dotted line), respectively. All ADCs were calculated with maximum b value of 800 sec/mm2. The midline of each box shows the median value, and the box extends from first to third quartiles. The whiskers extend from the first and third quartiles to the smallest and largest values, respectively, if those values are within 1.5 times the IQR. If not, the length of the whiskers is limited to 1.5 times the IQR. Image courtesy of the RSNA.
Apparent diffusion coefficient (ADC) measurements for benign and malignant BI-RADS category 4 or 5 lesions at MRI. (A, B) Benign BI-RADS category 4 lesion in a 55-year-old woman. (A) Dynamic contrast-enhanced MRI (DCE-MRI) scan shows a 12-mm, oval, circumscribed, homogeneous mass in the right posterior breast (arrow). (B) On the diffusion-weighted image, the lesion shows high diffusivity (arrow), with an ADC of 2.04 × 10-3 mm2/sec. Biopsy revealed benign fibroadenoma. (C, D) Malignant BI-RADS category 4 lesion in a 41-year-old woman. (C) DCE-MRI scan shows a 24-mm irregular, heterogeneous mass at the 3 o’clock position in the left breast (arrow). (D) On the diffusion-weighted image, the lesion demonstrates low diffusivity (arrow), with an ADC of 0.91 × 10-3 mm2/sec. Biopsy revealed invasive ductal carcinoma. All MRI scans are shown in the axial plane. (E) Box plot shows ADC measurements for 240 BI-RADS 4 and 5 lesions (63 malignant and 177 benign). Both prespecified optimal and conservative ADC cutoffs are indicated on the plot for reference: 1.53 × 10-3 mm2/sec (dashed line) and 1.68 × 10-3 mm2/sec (dotted line), respectively. All ADCs were calculated with maximum b value of 800 sec/mm2. The midline of each box shows the median value, and the box extends from first to third quartiles. The whiskers extend from the first and third quartiles to the smallest and largest values, respectively, if those values are within 1.5 times the IQR. If not, the length of the whiskers is limited to 1.5 times the IQR. Image courtesy of the RSNA.
The researchers tested the validity of point-of-care ADC measurements with the trial’s cutoff, with the goal of reducing unnecessary biopsies in lesions found by breast MRI. They included data from consecutively performed MRI exams from 2015 to 2019 at a single center. The exams showed biopsy-confirmed lesions at BI-RADS 4 or 5.
The team calculated sensitivity and biopsy reduction rates by applying the A6702 optimal (ADC, 1.53 × 10−3 mm2/sec) and alternate conservative (1.68 × 10−3 mm2/sec) cutoffs. The study included 240 breast lesions in 201 women with an average age of 49. Of the total lesions, 63 were deemed malignant while 177 were benign.
Applying the optimal cutoff led to a greater biopsy reduction rate compared to the conservative cutoff, albeit with lower sensitivity.
| Comparison between ADC cutoffs in biopsy reduction | ||
|---|---|---|
| Conservative cutoff | A6702 optimal cutoff | |
| Sensitivity | 95.2% | 92.1% |
| Biopsy reduction rate | 10.4% | 15.8% |
The researchers also found a higher sensitivity for masses (100%) than for nonmass enhancements (85.3%, p = 0.009) when applying the optimal cutoff. They reported comparable results for screening versus diagnostic examinations (p = 0.92 and 0.4, respectively).
Finally, repeated single-reader measurements showed good agreement with clinical ADCs, including an intraclass correlation coefficient of 0.72.
The study authors suggested that DWI performance could be further improved via more specific training and greater distribution of standardized ADC measurement methods and cutoffs.
“In the future, larger studies should be conducted to investigate the rates of lesion DWI non-evaluability and performance in different malignant subtypes,” they added.
In an accompanying editorial, Maya Honda, MD, PhD, from Kansai Electric Power Hospital, and Mami Iima, MD, PhD, from Kyoto University, wrote that ADCs could serve in a complementary role for dynamic contrast-enhanced MRI (DCE-MRI) in reducing unnecessary biopsies.
They added that other advanced diffusion MRI approaches could help provide information on tumor vascularization and the tumor microenvironment, and that combining other sequences or modalities could help identify other forms of breast cancer.
“Continued efforts in qualification and quantification could potentially provide assistance in avoiding overdiagnosis while improving diagnostic accuracy,” Honda and Iima wrote.
The full study can be found here.