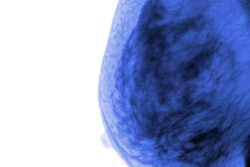
Benign breast disease diagnosed through percutaneous biopsy increases the overall risk of developing breast cancer, according to research published December 13 in JAMA Surgery.
A team led by Dr. Mark Sherman from the Mayo Clinic in Jacksonville, FL, found that presence of the disease on percutaneous biopsy is tied to a similar degree of increased breast cancer risk compared with surgically diagnosed benign breast disease. It also reported that the risks of both invasive breast cancer and ductal carcinoma in situ (DCIS) remained elevated among patients with the disease compared with the general population.
“The findings suggest that opportunities to improve breast cancer risk stratification exist for women with benign breast disease,” the Sherman team wrote.
Benign breast disease makes up about 75% of breast biopsy diagnoses. Surgical biopsy specimens diagnosed as nonproliferative, proliferative disease without atypia, or atypical hyperplasia are linked to increased breast cancer risk.
However, Sherman and colleagues pointed out that there is little data knowledge on risk associated with benign breast disease diagnosed via percutaneous biopsy, something they estimated in their current study.
The team collected benign breast disease biopsy specimens from 2002 to 2013, which were reviewed by two pathologists. The women underwent follow-up mammography exams from six months after biopsy until censoring, breast cancer diagnosis, or the cutoff date of December 31, 2021. The team also compared breast cancer risk in patients with benign breast disease with female breast cancer incidence rates from the Iowa Surveillance, Epidemiology, and End Results (SEER) program.
The study included data from 4,819 women with a median age of 51. Median follow-up was 10.9 years for women in the control group without breast cancer and 6.6 years for women with breast cancer.
The researchers found that standard incidence ratios, indicating risk, were higher in women with benign breast disease than in the control women in the SEER cohort.
Breast cancer findings were compared to health controls in SEER data, with a standard incidence ratio of 1 as the reference. Benign breast disease findings on biopsy were compared to surgical cohorts with benign breast disease, with a standard incidence ratio with 1 as the reference.
Benign breast disease diagnoses and outcomes |
Standard incidence ratio (with 1 as reference) |
|---|---|
| Overall breast cancer | 1.95 |
| Invasive breast cancer | 1.56 |
| DCIS | 3.10 |
| Increased benign breast disease for nonproliferative biopsy findings | 1.42 |
| Proliferative disease without atypia | 2.19 |
| Atypical hyperplasia | 3.91 |
The researchers also reported that the 10-year breast cancer cumulative incidence was 4.3% for nonproliferative, 6.6% for proliferative disease without atypia, and 14.6% for atypical hyperplasia. Meanwhile, the expected population cumulative incidence was 2.9%.
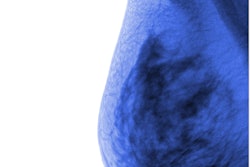
Finally, detection of multiple clusters of mammographic calcifications, a marker of multifocal benign breast disease, is tied to increased risk, the researchers reported.
“As 36.3% of breast cancers diagnosed after benign breast disease occurred in the contralateral breast and ipsilateral breast cancers among patients with prior benign breast disease diagnoses often develop in a different quadrant, understanding [disease] multiplicity may be important for risk prediction,” they wrote.
Based on these findings, current clinical management of benign breast disease in the percutaneous biopsy era should remain the same, the study authors suggested. This includes close surveillance through mammography and consideration of preventive therapy for women with atypical hyperplasia.
In an accompanying editorial, authors led by Julie Dalton from Duke University Medical Center in Durham, NC, wrote that while the generalizability of the data should be considered, the Sherman team’s study highlights the question of how a more objective approach should be implemented for individual risk assessment. They suggested that advancements in imaging and genetics may direct future risk assessments and management recommendations.
“Recent developments in mammography artificial intelligence algorithms may allow for better detection of high-risk features and prediction of breast cancer using only imaging,” they wrote. “Alternatively, rapidly evolving genomic assays, such as polygenic risk scores, may also further refine risk estimates.”