Deep feature extraction and MRI radiomics can help predict survival in breast cancer patients treated with neoadjuvant chemotherapy, according to research published November 17 in Academic Radiology.
Investigators led by doctoral candidate Quan Yuan of the Harbin Medical University Cancer Hospital in Heilongjiang, China, found that their model, which integrated imaging, pathology, and clinical data, achieved high marks in predicting overall five- and seven-year survival for women undergoing chemotherapy.
“This represents a meaningful advancement over existing models that rely on single-modality data or focus on short-term outcomes,” the Yuan team wrote.
While neoadjuvant chemotherapy is the standard treatment for early-stage breast cancers, outcomes may vary due to variability between patients. This is due to inherent heterogeneity in tumor biology, the researchers noted.
“This underscores an urgent need for more precise prognostic tools to optimize clinical decision-making,” they added.
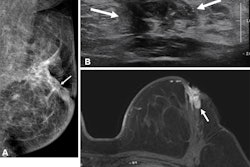
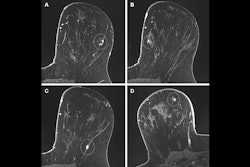
Yuan and colleagues developed a multimodal model that integrated deep feature representations and radiomic variables from clinical characteristics, pathomic features, deep learning-derived pathological features, and multiparametric MRI radiomics.
The multicenter study included 216 women with breast cancer who completed neoadjuvant chemotherapy and with no overlap in datasets with previous research. The team randomly divided the patient data into training and test sets at a 7:3 ratio for internal model construction and validation.
Compared with single-modality models, the multimodality model achieved superior performance for the most part in terms of area under the curve (AUC).
Performance of models in predicting overall survival (AUC) | |||||
Overall survival | MRI model | Pathomic model | Deep-learning pathomic model | Deep feature-based patho-radiomic model (training set) | Deep feature-based patho-radiomic model (test set) |
5-year | 0.66 | 0.69 | 0.86 | 0.89 | 0.82 |
7-year | 0.78 | 0.73 | 0.86 | 0.91 | 0.87 |
On Kaplan-Meier curve analysis, the team reported that the following factors did not have any statistical significance in predicting overall survival in these patients: estrogen receptor status, human epidermal growth factor receptor 2 (HER2) status, progesterone receptor status, and triple-negative breast cancer (TNBC) status.
Also, the performance of clinical characteristics showed inferior performance, with AUCs for five-year overall survival ranging from 0.4 to 0.53 and AUCs for seven-year overall survival ranging from 0.45 to 0.53, respectively. These included clinical characteristics such as pathological complete response, tumor size and staging, and lymph node status.
Finally, the deep feature-based patho-radiomic model showed the highest net benefit in the training set predicting five-year and seven-year overall survival. This applied when the threshold probability on calibration curve analysis is less than around 0.3.
The study authors suggested that the model’s success “likely” stems from its ability to capture both macroscopic tumor burden and microscopic biological behavior.
They also called for prospective studies to assess whether treatment guided by the multimodal model improves patient outcomes.
Read the full study here.