Diffusion-weighted MRI (DWI-MRI) helps in selecting ovarian cancer patients fit for primary debulking surgery, according to research published May 17 in Gynecologic Oncology.
Researchers led by Dr. Zheng Feng from Fudan University Shanghai Cancer Center in China found that DWI-MRI has good diagnostic performance in evaluating ovarian cancer prior to surgery.
"[These results] expand the application of [DWI-MRI] as an image technique for the preoperative predictive models," Feng and co-authors wrote.
While primary debulking surgery is considered the standard surgical treatment strategy for women with ovarian cancer, neoadjuvant chemotherapy may also be considered for women who may be considered as poor surgical candidates. Laparoscopic evaluation has "great diagnostic value" for assessing cancer, but the researchers noted that patients may refuse this strategy due to increased costs and its invasive nature.
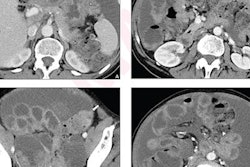
Previous studies suggest that DWI-MRI has high accuracy by providing high signal intensities of structures with water movement restriction, as well as "almost no" signal from other anatomical structures. Past research also suggests this modality has higher diagnostic accuracy than CT when assessing ovarian cancer.
The university's cancer center uses two validated predictive models. These include a noninvasive model by CT scans according to clinic-radiological criteria set by Suidan et al in a 2017 study, and a minimally invasive model that goes by the Fagotti laparoscopic score.
Feng and colleagues wanted to evaluate the value of DWI-MRI in selecting ovarian cancer patients who would benefit from primary debulking surgery. It also wanted to explore the cutoff value for the Suidan criteria at the team's cancer center. These criteria consisted of clinical and CT data tied to residual disease to predict surgical outcomes. The researchers applied DWI-MRI to the criteria for this study.
The Fagotti score meanwhile predicts the chances of optimal cytoreductive surgery in advanced ovarian cancer patients. It uses seven criteria points, each of which is assigned a predictive index value of 0 to 2. The total score ranges from 0 to 14, with lower scores indicating a higher likelihood of cytoreductive surgery.
The idea for the study is that these two approaches could help when triaging ovarian cancer patients for best treatment options.
The researchers included prospective data from 80 ovarian cancer patients with primary debulking surgery. Of these, 78 women were at an advanced stage while 72 had high-grade serous ovarian histology. Additionally, 46 women had no residual disease (R0), and 27 had optimal debulking surgery with macroscopic disease less than or equal to 1 cm (R1).
Also, patients with BRCA1 mutation had a lower R0 resection rate (42.9% vs. 63.0%) and a higher R1 resection rate compared with wild-type patients (50% vs. 29.6%).
The team found that the median predictive Fagotti score was 4. Also, the Suidan criteria with DWI-MRI had an area under the curve (AUC) of 0.742. To compare, the 2017 Suidan study using CT had an AUC of 0.548.
Using their DWI-MRI method, the researchers also found that the R0 resection rates for patients with predictive scores of 0 to 2, 3 to 5, and 6 or higher were 77.8%, 62.5%, and 23.8%, respectively. They wrote that the lower R0 resection rates may be because of the higher tumor burden of the patients.
The study authors wrote that based on their results, a cutoff Fagotti score of 5 is recognized as the cutoff value to discriminate surgical candidates. However, they noted that multi-center cooperation is still needed to establish the general criteria. Still, they highlighted that this personalized approach of using criteria from DWI-MRI and laparoscopic findings could successfully triage ovarian patients into different treatment approaches with elevated radical resection rates.