Research presented at ECR 2024 suggests that diffusion-weighted MRI (DW-MRI) has value in ovarian cancer treatment planning.
In his talk, Max Lahaye, MD, PhD, from the Netherlands Cancer Institute in Amsterdam discussed his team's findings which showed that DW-MRI could perform a complete primary and interval debulking with high accuracy.
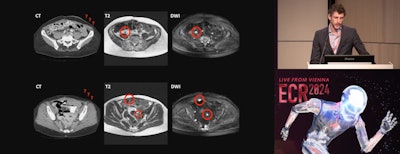 Max Lahaye, MD, of the Netherlands Cancer Institute in Amsterdam presents findings on the clinical impact of dedicated MR staging of ovarian cancer patients during ECR 2024.
Max Lahaye, MD, of the Netherlands Cancer Institute in Amsterdam presents findings on the clinical impact of dedicated MR staging of ovarian cancer patients during ECR 2024.
The Netherlands Cancer Institute, Leiden University Medical Center, and Catharina Ziekenhuis Teaching Hospital are collaborating on the multicenter MISSION trial. Part of the trial's overarching work includes predicting whether complete debulking surgery could be achieved and whether or not DW-MRI could be a cost-effective method in the diagnostic work-up of advanced ovarian cancer.
The researchers designed their prospective study to follow a routine care path. The study also evaluated surgical outcomes, interobserver agreement, and whether MRI could depict small lesions not detected during the initial surgical inspection.
The study included 220 advanced-stage (FIGO III/IV) ovarian cancer patients ages 65 to 67 who were scheduled for primary (n = 27) or interval (n = 193) debulking between 2018 and 2023. Anyone with contraindications for debulking or MRI, and no prior malignancy up to five years before surgery, was excluded.
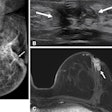
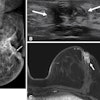
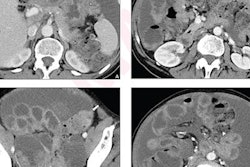
Although surgeons use a scoring system called a peritoneal cancer index (PCI) to divide the abdomen into 13 regions and measure the extent of disease, Lahaye's research showed that a special step in a surprise preoperative DW-MRI scan was especially useful.
"We have quite a simple MRI protocol: T2-weighted images, T1 pre- and postcontrast, and of course diffusion-weighted images," Lahaye said. "And I can't stress this enough: People have to drink one liter of pineapple juice because this will result in a nice quality because it will suppress the high signal on the diffusion-weighted images in the bowel. Because I don't want to see bowels, I want to see cancer. So please, use pineapple juice when you use these protocols."
Lahaye added that surgeons were not informed about the preoperative MRI and did not have an opportunity to see the MRI results until after they had inspected the whole abdomen and evaluated a PCI score.
Lahaye's team found that MRI could predict a complete primary and interval debulking and did so "quite accurately" in the primary group (AUC 0.9) and in the interval group (AUC 0.83). He cautioned, though, that for lesions below 4 mm MRI will still struggle to see them. Lahaye also noted good interobserver agreement (0.81).
In addition, after seeing the DW-MRI imaging data, surgeons confirmed MRI findings that they missed in their initial surgical inspection. Finally, the team concluded that MRI appeared to be budget-neutral as a result of ruling out diagnostic laparoscopy in some cases.
"Complete debulking is very important ... that every visible disease has to be removed surgically," Lahaye said. "But in the Netherlands, it's almost futile surgery."
And while diagnostic laparoscopy works well in predicting a complete debulking, Lahaye said this is not ideal.
"We as radiologists have a problem in depicting disease on CT, peritoneal disease. We have a sensitivity of 11% for lesions smaller than 5mm. That's really low. While on MRI, especially on diffusion-weighted images, these lesions light up like a lightbulb," he said.
Lahaye concluded that this research is important because patients with advanced disease have a poor five-year prognosis as ovarian cancer is often detected too late, at end-stage, by the time of diagnosis.
For more coverage from ECR 2024, please visit our RADCast.



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)