An MRI measurement of liver fat is strongly associated with the odds of prediabetes and type 2 diabetes in obese patients, according to a study published October 21 in Radiology.
In an analysis of 683 patients with obesity, each incremental increase in liver proton density fat fraction was associated with progressively higher odds of prediabetes and overt diabetes, noted lead author Ming Deng, MD, of Wuhan University in Wuhan, China, and colleagues.
“Our study demonstrated a robust, validated, and dose-dependent association between liver proton density fat fraction (PDFF) and the risk of diabetes in individuals with obesity,” the group wrote.
Metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as nonalcoholic fatty liver disease, is rising globally in parallel with obesity and type 2 diabetes, the authors explained. MASLD increases the risk of progressive liver diseases, but also contributes to metabolic dysregulation, particularly type II diabetes development, they added.
That's why precise risk stratification methods are urgently needed to manage these patients, and while MRI-based PDFF is an established tool for diagnosing fatty liver (liver steatosis), its role in predicting dysglycemia in obese individuals remains underexplored, the researchers noted.
The group conducted a retrospective analysis of 683 adult patients with obesity who underwent MRI to determine PDFF and who were administered an oral glucose tolerance test. Based on the glucose tolerance test results, the researchers classified patients as having normal glucose tolerance, prediabetes, or type 2 diabetes. Next, they categorized patients’ steatosis severity by PDFF (<5%, 5% to <15%, 15% to <25%, or ≥25%) and assessed associations between liver PDFF and prediabetes or type 2 diabetes.
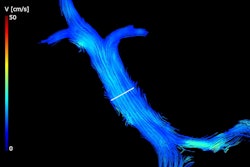
![Axial proton density fat fraction (PDFF) maps show hepatic steatosis assessment in patients with dysglycemia. (A) PDFF map in a 27-year-old female patient (body mass index [BMI; calculated as weight in kilograms divided by height in meters squared] = 38.9) with a 1-year history of obesity and metabolic syndrome, and hospital-confirmed prediabetes. The image shows moderate hepatic steatosis (mean liver PDFF, 19%; circle). (B) PDFF map in a 40-year-old male patient (BMI = 33.35) with a history of obesity, metabolic syndrome, hypertension, and hospital-confirmed type II diabetes. The image shows severe hepatic steatosis (mean liver PDFF, 40%; circle).](https://img.auntminnie.com/mindful/smg/workspaces/default/uploads/2025/10/pdff.not9GYHJg1.jpg?auto=format%2Ccompress&fit=max&q=70&w=400) Axial proton density fat fraction (PDFF) maps show hepatic steatosis assessment in patients with dysglycemia. (A) PDFF map in a 27-year-old female patient (body mass index [BMI; calculated as weight in kilograms divided by height in meters squared] = 38.9) with a 1-year history of obesity and metabolic syndrome, and hospital-confirmed prediabetes. The image shows moderate hepatic steatosis (mean liver PDFF, 19%; circle). (B) PDFF map in a 40-year-old male patient (BMI = 33.35) with a history of obesity, metabolic syndrome, hypertension, and hospital-confirmed type II diabetes. The image shows severe hepatic steatosis (mean liver PDFF, 40%; circle). RSNA
Axial proton density fat fraction (PDFF) maps show hepatic steatosis assessment in patients with dysglycemia. (A) PDFF map in a 27-year-old female patient (body mass index [BMI; calculated as weight in kilograms divided by height in meters squared] = 38.9) with a 1-year history of obesity and metabolic syndrome, and hospital-confirmed prediabetes. The image shows moderate hepatic steatosis (mean liver PDFF, 19%; circle). (B) PDFF map in a 40-year-old male patient (BMI = 33.35) with a history of obesity, metabolic syndrome, hypertension, and hospital-confirmed type II diabetes. The image shows severe hepatic steatosis (mean liver PDFF, 40%; circle). RSNA
“These findings underscore the clinical significance of quantifying liver PDFF, even at mild stages, in this high-risk population,” the researchers wrote.
By quantifying PDFF values, even at low levels of steatosis, radiologists can gain clinically actionable information that will help guide patient management and prevention, the researchers suggested.
To advance this application, however, longitudinal studies integrating PDFF with multiomics are warranted, they concluded.
In an accompanying editorial, Scott Reeder, MD, PhD, and Jitka Starekova, MD, of the University of Wisconsin-Madison, wrote that the study provides valuable data suggesting that fat accumulation in the liver, rather than being a passive process, may be a key driver of insulin resistance and subsequent development of diabetes.
“This study marks an important contribution, providing both a strong foundation for future research and a compelling case for the broader clinical adoption of PDFF,” Reeder and Starekova wrote.
The full study is available here.