An MRI technique that uses xenon-129 (Xe-129) gas shows lower ventilation and gas exchange in the lungs of individuals with long-term COVID-19 symptoms compared with healthy people, a study published June 28 in Radiology has found.
The results suggest that MRI could offer clinicians a useful alternative to CT for assessing COVID-19 patients going forward, especially as these long-term symptoms can be subtle, wrote a team led by Alexander Matheson, a doctoral student at Western University in London, Canada.
"Because MRI directly probes the function of the alveolar-capillary boundary, it may be more sensitive or more targeted than CT to microvascular abnormalities," the group noted.
Previous studies have indicated that the incidence of post-COVID-19 symptoms among people who are at least 12 weeks out from initial infection -- such as labored breathing at both rest and on exertion, fatigue, exercise limitation, muscle weakness, and cognitive deficits (i.e., "brain fog") -- ranges from 20% to 81%, the investigators explained.
These symptoms can be difficult to identify and treat as they often can't be consistently confirmed by tools such as spirometry, pulmonary tests, or even CT exams. Also, previous research has investigated the long-term effects of COVID-19 in patients who were hospitalized for it, not in those who were never hospitalized.
Xe-129 MRI offers the ability to identify "capillary-level abnormalities by detecting inhaled Xe-129 dissolved in the alveolar membrane," the group wrote. Matheson and colleagues explored any links between persistent COVID-19 symptoms and exercise limitations in 34 patients who contracted COVID-19 but were never hospitalized using Xe-129 MRI and CT pulmonary vascular measurements. Their study also included six healthy controls.
Patients with post-acute COVID-19 syndrome underwent spirometry, a lung test called diffusing capacity of the lung for carbon monoxide (DLCO), Xe-129 MRI, and chest CT, while the healthy controls had each of these tests except for chest CT.
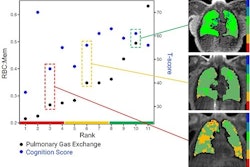
The team tracked patients' Xe-129 MRI exam red blood cell to alveolar-barrier signal ratios and red blood cell areas under the curve (AUC) values. Study participants also completed a variety of questionnaires to assess their quality of life, exercise limitations, and labored breathing.
The Xe-129 gas MRI exams showed poorer values in lung health measures such as the lungs' diffusing capacity for carbon monoxide, exercise capacity, and ease of breathing (conditions that were related to Xe-129 MRI findings on what the team labeled "red blood cell area under the spectroscopy curve," calling it "AUC"). The MRI findings also correlated with poor CT exam pulmonary vascular density findings.
"In our study, [Xe-129 MRI suggests] temporally persistent pulmonary vascular density and gas-transfer abnormalities that were related to exercise limitation and exertional dyspnea," the investigators wrote. "We observed abnormal Xe-129 MRI gas-exchange measurements in never-hospitalized participants with COVID, and some Xe-129 MRI measurements were worse in never-hospitalized patients compared with controls."
The findings show promise, but the study does have a few limitations: Namely, the method by which the Xe-129 MRI exams were conducted and what it showed about gas transfer, and age differences between healthy and patient participants, wrote Jim Wild, PhD, and Guilhem Collier, PhD, both of the University of Sheffield in the U.K., in an accompanying editorial.
"We are really pleased to see this work adding to the literature on dissolved xenon MRI in post-COVID lung disease and share the urgency to understand post-COVID lung disease symptoms," they wrote. "We do however need to make sure that the findings sit sensibly with appropriately age-matched normative data before clinically meaningful conclusions can be drawn."




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











