CHICAGO - While having a way to go, ultrafast breast MRI has potential to predict upstaging of ductal carcinoma in situ (DCIS) lesions, suggests research presented November 27 at the RSNA annual meeting.
Dr. Rachel Miceli from New York University (NYU) Langone Health presented the study, which showed that one feature from this method, time to enhancement (TTE), can be a predictive marker separating DCIS from invasive cancer.
"This showed some promising early data from a retrospective study, that TTE can help predict DCIS lesions that would be upgraded," Miceli said.
While DCIS has an upgrade rate of 0% to 59%, several risk factors have been identified in upstaging DCIS to invasive breast cancer. These include high-grade biopsy pathology, large lesion size, and suspicious imaging features. Sentinel lymph node biopsy, meanwhile, isn't typically indicated, Miceli noted.
However, TTE, which represents the amount of time from aortic enhancement to lesion enhancement, has been linked with aggressive lesion features. A shorter TTE usually means invasive cancer.
Miceli and colleagues wanted to find out whether ultrafast MRI kinetic features are linked to biopsy-proven DCIS upgrade after surgical excision. They looked at data from 68 women with a median age of 52 years who had biopsy-proven DCIS and who went through preoperative conventional dynamic contrast-enhanced (DCE)-MRI with ultrafast. They also looked at patient characteristics, biopsy parameters and biopsy pathologies, DCE-MRI lesion characteristics, and ultrafast MRI features.
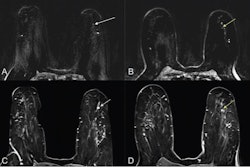
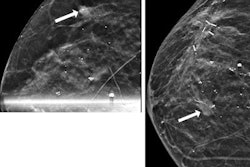
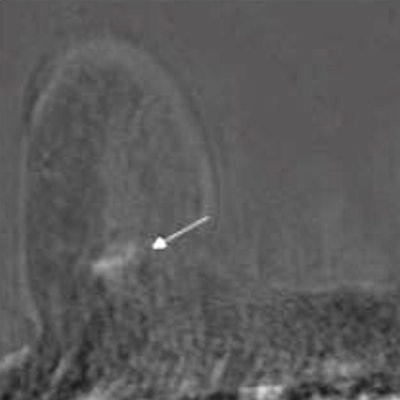
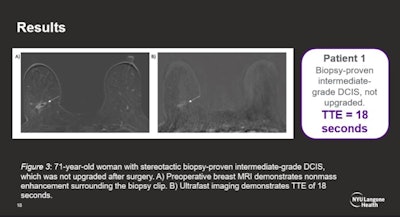 Ultrafast MRI images have potential to predict upstaging of DCIS lesions by measuring time to enhancement (TTE), according to research presented at the RSNA annual meeting. Image courtesy of Dr. Rachel Miceli.
Ultrafast MRI images have potential to predict upstaging of DCIS lesions by measuring time to enhancement (TTE), according to research presented at the RSNA annual meeting. Image courtesy of Dr. Rachel Miceli.The researchers found that out of the total, seven DCIS lesions (11%) were upgraded to higher-grade DCIS. Another 26 lesions (38%) were upgraded to invasive cancer.
Also, upgrade to invasive cancer was significantly tied to shorter TTE on preoperative ultrafast MRI (p = 0.031). This includes an optimal threshold of 11 seconds, with 50% specificity and 76% sensitivity for upgrade. This is consistent with previous studies on TTE time. The team also found that needle gauge size (p = 0.049) and larger lesion size (p = 0.001) were linked to upgrade from DCIS to invasive cancer, with an optimal threshold of 4.35 cm.
However, the study authors also reported that no other parameters or patient characteristics were linked to DCIS upgrade after surgery. Finally, logistic regression for size and TTE combined in predicting upgrade showed a higher area under the curve (0.76) than each factor alone, but this did not achieve statistical significance.
While ultrafast MRI did not achieve its goals, Miceli said the study shows promise that TTE can potentially help upgrade DCIS lesions. She added that better predictability can perhaps pave the way for this method to help surgeons with decision-making.
"I think if we have more cases and maybe add more variables, maybe from mammograms or ultrasounds, we may be able to hopefully get the sensitivity and specificity higher," she said. "This should be investigated in a larger sample size."