MR spectroscopy imaging can effectively distinguish between recurrent brain tumors and necrosis in patients who have undergone radiation treatment, a study published January 11 in the Journal of Neuroimaging has found.
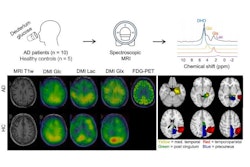
The technique measures the biomarkers Cho/NAA (choline/N-acetyl-aspartate), Cho/Cr (choline/creatine), and NAA/Cr (N-acetyl aspartate/creatine) -- which can help differentiate between recurrent disease and necrosis, wrote a team led by Dr. Almusaedi Aseel of National University of Ireland in Galway.
"[Our review found that the MR spectroscopy imaging exam] is a safe, accurate, and informative tool for distinguishing between the two diagnostic entities," the authors noted.
Necrosis after brain cancer radiation treatment is a serious consequence to treatment, and it tends to manifest within six months, the team noted. MRI spectroscopy has been used to identify brain tumors, and Aseel's team sought to determine if it could distinguish between necrosis caused by radiation treatment and recurrent brain tumors. The technique suppresses the water signal on MRI and matches spectral signals from different molecules to tumor biology, the group explained.
"The application of [MR spectroscopy imaging] in brain tumors continues to be a promising area of advancement in brain tumor management with significant benefits in the context of different physiological imaging techniques," the authors wrote.
To assess MR spectroscopy imaging's effectiveness for distinguishing between recurrent brain cancer and necrosis, Aseel and colleagues conducted a literature review that included nine papers with data from 354 patients that were published between 2011 and 2021. The papers explored MR spectroscopy imaging's ability to track and quantify the biomarkers.
The review found that, out of the nine studies, five showed strong significance of Cho/NAA and Cho/Cr ratios in distinguishing between recurrent tumors and necrosis, and four indicated that the NAA/CR ratio also accomplished this. One study emphasized that MR spectroscopy imaging helps clarify indefinite, suspicious symptoms found on follow-up MRI.
"[MR spectroscopy imaging] using Cho/Cr and Cho/NAA ratios allows for a noninvasive distinction between relapsed gliomas and radiation damage in patients with indeterminate prognosis on routine follow-up," the group explained.
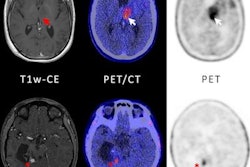
Aseel's team acknowledged that there are other ways to distinguish between recurrent brain cancers and radiation-induced necrosis, including PET, SPECT, diffusion-weighted MRI, and MRI perfusion, but noted that determining which of these is best for this application can be tricky.
"Most published articles conclude that a pursuit of a combination of techniques might be the only way to raise diagnostic accuracy," the investigators wrote.
In any case, MR spectroscopy imaging is a solid tool for evaluating suspicious findings in brain cancer patients after radiation treatment.
"The application of MR spectroscopy imaging in brain tumors continues to be a promising area of advancement in brain tumor management with significant benefits in the context of different physiological imaging techniques, including diffusion tensor, diffusion-weighted, and dynamic contrast-enhanced MRI," the authors concluded.