Percent insular ribbon infarction (PIRI) on MRI helps classify patients with slowly progressive stroke who could benefit from late-window endovascular thrombectomy (EVT), a study published February 15 in the American Journal of Roentgenology has found.
Researchers led by Dr. Robert Regenhardt, PhD, from Massachusetts General Hospital found that PIRI showed strong diagnostic performance in outcome prediction and could complement current prognostic and treatment strategies for patients with acute ischemic stroke.
"Patients with different PIRI categories at presentation showed significant differences in infarct growth rate at multiple time points," Regenhardt and co-authors wrote. "In addition, the PIRI category showed significant independent associations with infarct volumes and infarct growth rates up to 48 hours after presentation as well as with 90-day outcomes."
EVT can be used to care for patients with large-vessel occlusion (LVO) stroke, but over half of patients who receive this treatment have poor outcomes, previous reports suggest. The researchers also pointed out that delays often occur in transferring patients from community hospitals to EVT-capable centers, reducing the likelihood of the procedure being performed. This could be helped by better identifying patients with LVO stroke who could benefit from late-window EVT.
Infarct growth rate has been explored as a determinant of clinical outcomes after EVT, with several factors determining such rates of stroke. Another previous study showed that a five-point score measuring PIRI, which describes the extent of existing insular injury, may relate to stroke progression.
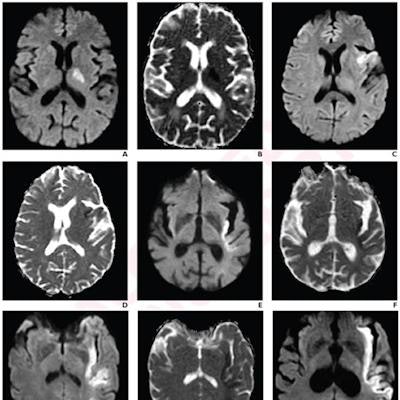
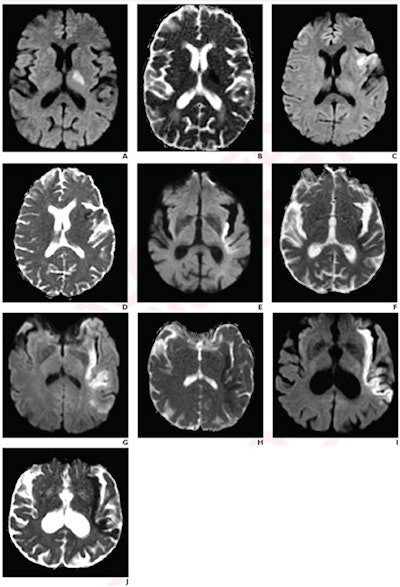 Images represent acute ischemic stroke patients with each PIRI score on a five-point scale. (A) Diffusion-weighted imaging (DWI) and (B) apparent diffusion coefficient (ADC) mapping show a 71-year-old patient with 0% insular ribbon infarction, score 0. (C) DWI and (D) ADC mapping show a 62-year-old patient with 25% insular ribbon infarction, score 1. (E) DWI and (F) ADC mapping show a 90-year-old with 50% insular ribbon infarction, score 2. (G) DWI and (H) ADC mapping show a 59-year-old with 75% insular ribbon infarction, score 3. (I) DWI and (J) ADC mapping show a 69-year-old with 100% insular ribbon infarction, score 4. Images courtesy of the American Roentgen Ray Society.
Images represent acute ischemic stroke patients with each PIRI score on a five-point scale. (A) Diffusion-weighted imaging (DWI) and (B) apparent diffusion coefficient (ADC) mapping show a 71-year-old patient with 0% insular ribbon infarction, score 0. (C) DWI and (D) ADC mapping show a 62-year-old patient with 25% insular ribbon infarction, score 1. (E) DWI and (F) ADC mapping show a 90-year-old with 50% insular ribbon infarction, score 2. (G) DWI and (H) ADC mapping show a 59-year-old with 75% insular ribbon infarction, score 3. (I) DWI and (J) ADC mapping show a 69-year-old with 100% insular ribbon infarction, score 4. Images courtesy of the American Roentgen Ray Society.In their research, Regenhardt and colleagues wanted to look at associations of PIRI with infarct growth rate during the initial 48 hours after presentation, as well as with 90-day outcomes, in patients with LVO stroke.
They evaluated data from 31 trial patients with a median age of 71 years. The patients had anterior-circulation LVO and underwent serial MRI examinations.
Two neuroradiologists independently scored PIRI on presentation MRI exams using a 0-to-4 scale. Scores were categorized as mild (0-1), moderate (2), or severe (3-4), and discrepancies were resolved by consensus. The radiologists had a strong inter-rater agreement for PIRI categories (k = 0.890).
The researchers found that PIRI was mild in 10 patients, moderate in four, and severe in 17. Also, infarct growth rate was significant in each time period.
| Infarct growth rate for PIRI categories at different time periods | ||||
| Median infarct growth rate time periods | Mild PIRI | Moderate PIRI | Severe PIRI | p-value |
| Onset-to-presentation (cc/h) | 1.6 | 8.5 | 17.5 | < 0.001 |
| Presentation-to-48 hours (cc/h) | 0.3 | 0.2 | 1.2 | 0.005 |
| 90-day infarct volume (cc) | 9.4 | 39.8 | 108.6 | 0.01 |
The researchers also found that the 90-day modified Rankin scale of score of two or less occurred in 78% with mild PIRI, 67% of patients with moderate PIRI, and 6% of patients with severe PIRI (p = 0.001). This scale measures disability in stroke patients.
They also looked at multivariable models controlling for age, internal carotid artery occlusion, and collateral pattern. The team found that PIRI categories independently predicted onset-to-presentation infarct growth rate (β = 1.5), presentation-to-48-hour growth rate (β = 1.3), and 90-day modified Rankin Scale of two or less (odds ratio = 0.2).
Finally, for predicting 90-day modified Rankin scale of two or less, mild-to-moderate PIRI had sensitivity of 90% and specificity of 84.2%. Symmetric collateral pattern had a sensitivity of 70% and specificity of 73.7%.
The study authors wrote that their findings indicate that PIRI at presentation offers predictive information beyond that obtained from other known predictors. They added that early insular infarction should serve as a "critical" early warning of subsequent poor outcomes in the absence of reperfusion.