
Biomarkers seen on cardiovascular MRI could guide management of systemic breast cancer treatment for women with ERBB2-positive disease, suggest findings published April 12 in JAMA Cardiology.
Researchers led by Dr. Paaladinesh Thavendiranathan from the University of Toronto found that particular MRI biomarkers show how inflammation and edema peak early during sequential anthracycline and trastuzumab therapy. They reported that these findings were associated with ventricular remodeling and B-type natriuretic peptide elevation but added that they are "transient."
"The changes were mostly small, on average within previously reported temporal variability, and overlapped between patients with and without cancer therapy-related cardiac dysfunction [CTRCD]," Thavendiranathan and colleagues wrote.
Current approaches to the challenge of identifying early myocardial injury from cancer therapy include measuring left ventricular volumes, myocardial strain, and serum biomarkers. However, the researchers noted that these approaches may detect injury at later stages. As such, there's growing interest in noninvasive early detection of myocardial tissue changes via cardiovascular MRI -- which could also measure risk for CTRCD. Recent animal studies support this hypothesis, but human data are limited, the authors noted.
Thavendiranathan and co-authors sought to explore any changes in cardiovascular MR tissue biomarkers during breast cancer therapy and their association with CTRCD. Specifically, they used MRI scans to describe longitudinal changes in myocardial tissue biomarkers that reflect inflammation, edema, and fibrosis. They collected data between 2013 and 2019 from 136 women. Of these, 37 (27%) developed CTRCD.
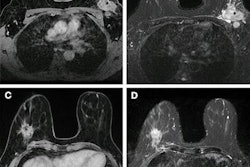
The team found that, compared with baseline, tissue biomarkers of myocardial hyperemia and edema peaked after anthracycline therapy or three months after the women started treatment with trastuzumab.
The group observed the following biomarker changes:
- Relative myocardial enhancement: gadolinium contrast material trickles into fibrotic or necrotic myocardial tissue.
- T1 and T2 mapping: Imaging maps generated at different degrees of longitudinal relaxation to receive a signal intensity versus time curve.
- Extracellular volume fraction, derived from T1 mapping: This reflects the size of the extracellular space in the myocardium.
The team did note that these changes were mostly within a normal range and returned to baseline levels during follow-up.
| Changes in biomarkers during breast cancer therapy as seen on cardiovascular MRI | ||
| Measure | Baseline | Peak |
| Relative myocardial enhancement | 46.3% | 56.2% |
| Native T1 mapping | 1,012 milliseconds | 1,035 milliseconds |
| T2 mapping | 51.4 milliseconds | 52.6 milliseconds |
| Extracellular volume fraction | 25.2% | 26.8% |
Among other findings the team reported, increases in T1 and T2 mapping, and extracellular volume fraction were associated with increased ventricular volumes and B-type natriuretic peptide. However, this trend did not go for high-sensitivity cardiac troponin I levels.
"None of the cardiovascular MR tissue biomarkers were associated with changes in left ventricular ejection fraction or myocardial strain," the researchers wrote. "Change in extracellular volume fraction was associated with concurrent and subsequent CTRCD, but there was significant overlap between patients with and without CTRCD."
The study authors suggested that while these findings may help future research that explores optimal timing for cardiac surveillance during cancer therapy, cardiovascular MR tissue biomarkers alone are "unlikely to be useful" at the patient level.
"Our findings may relate to the population studied as the patients in our study would be considered to be at low to medium risk of CTRCD as per recently published guidelines," they wrote. "Therefore, whether cardiovascular MR tissue biomarkers may have a diagnostic and prognostic value in patients at higher risk for cardiotoxicity remains to be studied."




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











