Infants with enlarged perivascular spaces have a more than two-fold greater chance of developing autism compared with infants with normal perivascular spaces, according to researchers from the University of North Carolina in Chapel Hill.
"These results suggest that perivascular spaces could serve as an early marker for autism," said study lead author Dea Garic, PhD, in a statement released January 2 by the university.
Every six hours, the brain expels a wave of cerebrospinal fluid (CSF) that flows through perivascular spaces; this fluid mitigates the buildup of neuroinflammatory proteins, such as amyloid beta. The cleansing process is especially efficient during sleep, and disruption of it can lead to neurological dysfunction, cognitive decline, or developmental delays, Garic's group explained.
Garic and colleagues conducted a study in conjunction with the Infant Brain Imaging Study (IBIS) (research that investigates brain development, autism, and related developmental disabilities and includes five universities, of which the University of North Carolina-Chapel Hill is the lead site), assessing infants at increased risk of autism due to having an older sibling with the condition and following them from six- to 24 months of age. The work included 870 MRIs that measured excessive CSF volume and enlarged perivascular spaces. MRI exams were obtained from babies during natural sleep at six, 12, and 24 months, the university said.
The group found that 30% of infants who later developed autism had enlarged perivascular spaces by 12 months, and by 24 months of age, nearly half of the infants diagnosed with autism had enlarged perivascular spaces. The findings were published in JAMA Network Open on December 19.
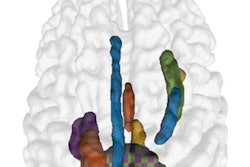
 Extra-axial cerebrospinal fluid (EA-CSF) and perivascular space (PVS) segmentation on a 24-month scan of a child who was diagnosed with autism. Image courtesy of Dea Garic, PhD, and Mark Shen, PhD.
Extra-axial cerebrospinal fluid (EA-CSF) and perivascular space (PVS) segmentation on a 24-month scan of a child who was diagnosed with autism. Image courtesy of Dea Garic, PhD, and Mark Shen, PhD.
"Since autism is so highly linked with sleep problems, we were in this unique position to examine CSF dynamics and sleep," Garic said. "It was really striking to observe such a strong association separated by such a long period of time over childhood. But it really shows how perivascular spaces not only have an effect early in life, but they can have long-term effects, too."
Excess CSF volume doesn't circulate through the brain as efficiently as it should, according to Garic. Going forward, the investigators plan to again use MR imaging to measure CSF in sleeping infants' brains, focusing on the physiology and speed of CSF flow. They are also working with colleagues to quantify the size of perivascular spaces and the severity of behavioral outcomes, and plan to extend their research to neurogenetic syndromes associated with autism, such as Fragile X syndrome and Down syndrome.
"Collectively our research has shown that CSF abnormalities in the first year of life could have downstream effects on a variety of outcomes, including later autism diagnosis, sleep problems, neuroinflammation, and possibly, other developmental disabilities," said senior author Mark Shen, PhD, in the university statement.
The complete study can be found here.