MRI shows that decreases in the brain's white matter and increases in ventricle volume are risk factors for the progression of mild cognitive impairment (MCI), according to a study published October 30 in JAMA Network Open.
A team led by Yuto Uchida, MD, PhD, of Johns Hopkins University School of Medicine in Baltimore found that these brain characteristics -- along with the presence of type 2 diabetes and abnormal beta-amyloid ratios in the cerebrospinal fluid (CSF) -- were associated with accelerated brain atrophy and an earlier progression to MCI.
"Our long-term longitudinal cohort study demonstrated considerable interindividual and intraindividual variations in annual rates of change in the whole-brain white matter volumes among individuals with unimpaired cognition at baseline," they wrote.
Risk factors that influence the trajectory from normal cognition to mild cognitive impairment are unclear, according to Uchida's group. The team conducted a study that examined factors associated with the acceleration of brain atrophy using longitudinal information from 185 middle-aged and older adults from the Biomarkers for Older Controls at Risk for Dementia (BIOCARD) database. BIOCARD began at the National Institutes of Health in January 1995 and continued there until December 2005; it was continued at Johns Hopkins between January 2015 to October 2023.
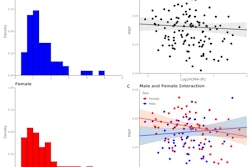
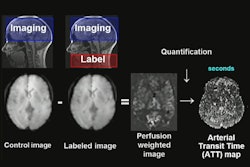
All participants in the BIOCARD trial were cognitively healthy at baseline. Uchida's team included data from participants whose structural MR imaging of the brain and CSF data were available over a 10-year span. The investigators tracked annual changes in segmental brain volumes, using Kaplan-Meier survival curves to plot time to MCI symptom onset and hazard ratios (with 1 as reference).
The researchers reported the following:
- Study participants with high levels of atrophy in the white matter and enlargement in the ventricles demonstrated earlier progression from normal cognition to MCI symptom onset (hazard ratio [HR] for white matter, 1.86, and for ventricles, 1.71).
- There was an association between type 2 diabetes and progression to MCI (HR, 1.41) and with low CSF beta-amyloid peptide 42 to beta-amyloid 40 ratio (HR, 1.48); the combination of both of these risk factors had an even higher HR of 1.55.
The study findings demonstrate that white-matter volume changes are "closely associated with cognitive function in aging, suggesting that white-matter degeneration may play a crucial role in cognitive decline," according to the authors.
"[Our] results support the importance of identifying individuals who have accelerated brain atrophy to optimize strategies to prevent MCI," they concluded.
The complete study can be found here.