A new method of MRI lung scanning shows the effects of treatment for compromised lung function in transplant patients, U.K. researchers have reported.
The method consists of using a special gas called perfluoropropane that can be seen on an MRI scanner, wrote a team led by Prof. Peter Thelwall, PhD, of Newcastle University in Newcastle on Tyne, U.K. The gas can be safely inhaled and exhaled by patients; MRI exams then show where in the lungs the gas has reached, according to the group. The findings were published December 24 in both Radiology and JHLT Open.
"Our scans show where there is patchy ventilation in patients with lung disease, and show us which parts of the lung improve with treatment," Thelwall said in a statement released by the university. "For example, when we scan a patient as they use their asthma medication, we can see how much of their lungs and which parts of their lung are better able to move air in and out with each breath."
The new technique could allow clinicians to quantify the degree of improvement in ventilation when patients have a treatment via an inhaler, and "could be valuable in clinical trials of new treatments of lung disease," the group noted.
For both publications, the researchers conducted studies for which they scanned transplant recipients' lungs with MRI over multiple inhales and exhales, collecting images that reveal how the air containing the gas reached different areas of the lung.
"In those with chronic rejection, the scans showed poorer movement of air to the edges of the lungs, most likely due to damage in the very small breathing tubes (airways) in the lung," they wrote.
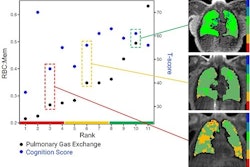
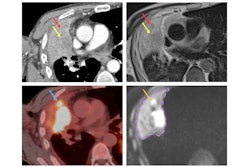
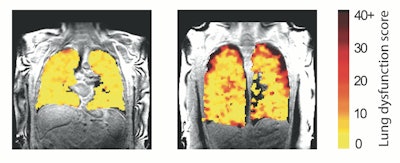 Lung function MRI showing problem areas (measurement levels of dysfunction) in lung transplant recipients.Image and caption courtesy of Newcastle University in Newcastle on Tyne, U.K.
Lung function MRI showing problem areas (measurement levels of dysfunction) in lung transplant recipients.Image and caption courtesy of Newcastle University in Newcastle on Tyne, U.K.
This scan method could be used to manage lung transplant recipients, "bringing a sensitive measurement that may spot early changes in lung function that enable better management of these conditions," according to the investigators.
"We hope this new type of scan might allow us to see changes in the transplant lungs earlier and before signs of damage are present in the usual blowing tests," said research co-author Prof. Andrew Fisher, PhD, also of Newcastle University. "This would allow any treatment to be started earlier and help protect the transplanted lungs from further damage."
The Radiology study can be found here and the JHLT Open study here.