An advanced type of MR imaging shows that children and adolescents with long COVID have significant lung abnormalities, according to a study published February 25 in Radiology.
The study findings "enhance our understanding of [long COVID] pathophysiologic structure and establish a foundation for future research," wrote a team led by Gesa H. Pöhler, MD, of Hannover Medical School in Germany.
"Further investigations should prioritize multicenter longitudinal studies with larger cohorts to validate these findings and evaluate the progression of lung abnormalities at various stages after COVID-19 infection," the group noted.
Long COVID can affect people of all ages and is diagnosed when symptoms continue more than 12 weeks after the initial infection, the investigators noted. Symptoms can include chronic fatigue, headaches, and poor concentration. Chest CT is often used to diagnose and monitor lung function of adults with the condition but is not recommended for children because it exposes them to radiation and may require a contrast agent. Children with suspected long COVID tend to be tracked with pulmonary function tests, echocardiography, and medical history review, but pulmonary function tests in particular may appear normal, even in patients manifesting symptoms.
Pöhler's team explored whether a technique called free-breathing phase-resolved functional lung (PREFUL) MRI -- which analyzes air movement in and out of the lungs and blood flow through the lungs, and doesn't require radiation or intravenous contrast -- could better image patients with long COVID. The group conducted a study between April 2022 and April 2023 that included 54 children between the ages of 11 and 17. Half of these children had been diagnosed with long COVID while the other half were healthy controls.
The researchers found that, compared to the healthy controls, children with long COVID had significantly reduced blood flow in the lungs, writing that "a reduction in blood flow patterns in organs or other areas of the body can result in a lack of sufficient oxygen and nutrients." All the long COVID patients except one reported fatigue.
"The severity of fatigue symptoms correlated with … blood flow changes, suggesting a possible biological basis for the patients' ongoing symptoms," Pöhler said in a statement released by the RSNA.
| Findings from PREFUL MRI in children without and with long COVID | |||
|---|---|---|---|
| Measure | Healthy controls | Participants with long COVID | p-value |
| Quantified perfusion | 78 mL/min per 100 mL | 49 mL/min per 100 mL | < 0.001 |
| Percentage of lung area not being ventilated (ventilation defect) | Median, 5.4% | Median, 7.6% | 0.047 |
| Perfusion defect percentage (size of a myocardial perfusion defect) | Median, 2.3% | Median, 3.2% | 0.02 |
Of the total cohort, 21 long COVID patients showed cardiopulmonary symptoms such as shortness of breath, and those with long COVID also demonstrated an association between greater lung perfusion and increased chronic fatigue severity (Pearson correlation coefficient [PCC] = 0.48; p = 0.009) and an association between higher ventilation-perfusion mismatch and increased heart rate (PCC = 0.44; p= 0.02).
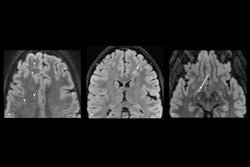
![Images show exemplary coronal sections of phase-resolved functional lung MRI defect maps in a pediatric participant with post-COVID-19 condition (PCC) and cardiopulmonary symptoms and a healthy control patient. (A) Images in a 17-year-old male participant with PCC show a ventilation defect percentage (VDP) of 17%, a perfusion defect percentage (QDP) of 16%, a ventilation/perfusion (V/Q) match healthy (VQM [H]) percentage of 64%, and a V/Q mismatch defect (VQM [D]) of 3%. (B) Images in a healthy control participant, with a ventilation defect percentage of 9%, a perfusion defect percentage of 5%, a V/Q match healthy percentage of 86%, and no V/Q mismatch defect. Images and caption courtesy of the RSNA.](https://img.auntminnie.com/files/base/smg/all/image/2025/02/2025_02_25_Radiology_Pohler_figure5.67be1584300b1.png?auto=format%2Ccompress&fit=max&q=70&w=400) Images show exemplary coronal sections of phase-resolved functional lung MRI defect maps in a pediatric participant with post-COVID-19 condition (PCC) and cardiopulmonary symptoms and a healthy control patient. (A) Images in a 17-year-old male participant with PCC show a ventilation defect percentage (VDP) of 17%, a perfusion defect percentage (QDP) of 16%, a ventilation/perfusion (V/Q) match healthy (VQM [H]) percentage of 64%, and a V/Q mismatch defect (VQM [D]) of 3%. (B) Images in a healthy control participant, with a ventilation defect percentage of 9%, a perfusion defect percentage of 5%, a V/Q match healthy percentage of 86%, and no V/Q mismatch defect. Images and caption courtesy of the RSNA.
Images show exemplary coronal sections of phase-resolved functional lung MRI defect maps in a pediatric participant with post-COVID-19 condition (PCC) and cardiopulmonary symptoms and a healthy control patient. (A) Images in a 17-year-old male participant with PCC show a ventilation defect percentage (VDP) of 17%, a perfusion defect percentage (QDP) of 16%, a ventilation/perfusion (V/Q) match healthy (VQM [H]) percentage of 64%, and a V/Q mismatch defect (VQM [D]) of 3%. (B) Images in a healthy control participant, with a ventilation defect percentage of 9%, a perfusion defect percentage of 5%, a V/Q match healthy percentage of 86%, and no V/Q mismatch defect. Images and caption courtesy of the RSNA.
The researchers wrote that children with long COVID should be monitored and that this tracking could help guide therapeutic interventions, with Pöhler noting that "quantitative lung MRI establishes a potential imaging biomarker profiling and helps to enable disease severity follow-up for this complex condition in the future."
In an accompanying editorial, Grace Parraga, PhD, of Western University in London, Canada, and Sarah Svenningsen, PhD, of McMaster University in Hamilton, Canada, agreed.
"Providing a way to 'see the unseen' certainly supports the argument to include MRI, and in particular PREFUL MRI, in children with challenging cases of [long COVID]," they concluded.
The complete study can be found here.