Researchers in Taiwan have devised a way to measure the severity of lower neck nerve injuries on preoperative MRI scans, according to a study published August 26 in Radiology.
The method involves measuring the volume of cervical paraspinal muscles and ultimately could help improve surgical treatments for patients, noted lead author Yun-Cong Zheng, MD, of National Taiwan University in Taipei City, and colleagues.
“Although breakthroughs in reconstructive microsurgery have led to improved clinical results for [traumatic brachial plexus injury], it requires precise diagnostic imaging classification to determine the appropriate surgical plan for achieving the desired outcomes,” the group wrote.
The brachial plexus is a network of nerves on either side of the lower neck that controls movement and sensation in the shoulders, arms, and hands. Blunt trauma to the site from motor vehicle accidents, for instance, can cause nerve roots to be cut or torn from the spinal cord and often requires surgery to repair, the researchers explained. Yet although cervical myelography, CT myelography, and MRI are commonly used to distinguish injured preganglionic roots from normal roots, they are not effective in differentiating between total and partial root avulsion, they added.
As the volume of muscles decreases as nerve stimulation decreases, the group sought to determine whether measuring paraspinal muscle volume, particularly in the deeper layers, could help determine the severity of nerve injury.
The researchers culled data from 145 patients (mean age, 30 years old) diagnosed with traumatic brachial plexus injury with upper limb weakness or paralysis. Patients had a preoperative MRI performed within one year of the injury and the severity of their root injuries were confirmed surgically.
To develop their method, the group labeled the muscles on the MR images according to injury side (right versus left), root level (C4 through C7), and layer depth (superficial to deep layers). Next, they devised an “L/N volume ratio” based on the difference in the segmented muscle volume on the injured side to that on the normal side. Lastly, they assessed whether the L/N volume ratio could differentiate the severity of root injury (normal roots, partial root avulsion, and total root avulsion) on the MRI reports.
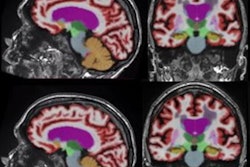
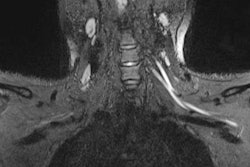
 Labeling of the four layers of paraspinal muscles on gadolinium-enhanced T1-weighted MRI scan in a 20-year-old man with left brachial plexus injury before surgery. Red numbers indicate the side with lesions, white numbers indicate the healthy side, and purple numbers indicate the vertebral body; the disk level within the intervertebral space represents the individual spinal root and nerve. RSNA
Labeling of the four layers of paraspinal muscles on gadolinium-enhanced T1-weighted MRI scan in a 20-year-old man with left brachial plexus injury before surgery. Red numbers indicate the side with lesions, white numbers indicate the healthy side, and purple numbers indicate the vertebral body; the disk level within the intervertebral space represents the individual spinal root and nerve. RSNA
The L/N volume ratio in layer 4 paraspinal muscles was higher in normal root injuries versus partial root avulsion (p < 0.001 for C4–C6, p = 0.16 for C7) and higher in partial root avulsion versus total root avulsion (p < 0.03 for C4–C7).
The L/N volume ratio cutoffs (0.95 and 0.80) enabled accurate distinction of normal from avulsed roots (area under the receiver operating characteristic curve [AUC], 0.88) and partial root avulsion from total root avulsion (AUC, 0.91).
The L/N volume ratio cutoffs enabled accurate diagnosis of all four roots (C4–C7) in 55.2% (80 of 145) of patients and three of four roots in 29% (42 of 145) of patients.
“MRI-based volumetric analysis of paraspinal muscles in patients with [traumatic brachial plexus injury] accurately distinguished the severity of root injury, which was associated with intraoperative findings,” the researchers concluded.
In an accompanying editorial, Darryl B. Sneag, MD, of Cornell University in New York City, and Falko Ensle, MD, of University Hospital Zurich in Switzerland, noted that the study elucidates the sensitive crosslink between nerve root injury severity and atrophy of the deep paraspinal muscle layer due to denervation.
While manual paraspinal muscle segmentation, as was performed in this study, may limit its widespread adoption in the clinical workflow, the rapid pace of development of AI algorithms for segmentation tasks promises to automate this process in the near future, they added.
“The study also inspires further research into applying quantitative MRI for muscle assessment in traumatic nerve injuries, potentially providing quantitative biomarkers to more precisely localize and grade injuries and predict treatment outcomes,” Sneag and Ensle concluded.
The full study is available here.