Use of the Gamma Knife stereotactic radiosurgery system as a treatment for cancer patients with recurring low-grade gliomas may help reduce recurring tumors and provide fair local control, according to findings presented at the recent 2008 RSNA meeting in Chicago.
In a study presented at the conference by radiation oncology resident Dr. Allison Quick, researchers performed a retrospective review of patients treated at the Arthur G. James Cancer Hospital of the Ohio State University Medical Center in Columbus.
Low-grade gliomas are a group of heterogeneous primary intracranial tumors that have a tendency to be diffusely infiltrative, recur frequently, and transform to higher-grade tumors. They consist of pilocytic astrocytomas at grade I on the World Health Organization (WHO) scale, and WHO grade II astrocytomas, oligodendrogliomas, and oligoastrocytomas.
"Management for low-grade gliomas remains controversial, but typically includes surgery, adjuvant external-beam radiation therapy, and possibly chemotherapy for a subset of patients," Quick explained. "Few studies have been published on the use of stereotactic radiosurgery, which is not a standard treatment for low-grade gliomas. The studies that have been published report local control rates with a range of 67% to 100%. We wanted to evaluate how the patients we treated ranked."
Quick and colleagues reviewed the charts of all patients who received stereotactic radiosurgery (Leskell Gamma Knife, Elekta, Norcross, GA) as a primary, secondary, or salvage therapy between 1999 and 2006. The team identified a total of 19 patients, 15 of whom received the treatment as salvage therapy after having already undergone surgery, radiation therapy, and/or chemotherapy. Two patients received the treatment as primary therapy and two as secondary therapy.
The patient cohort consisted of 12 males and seven females, ranging in age from 9 to 72 years, with a mean patient age of 38.9 years. Pathologic confirmation of a low-grade recurrence was made in only two of the 15 patients receiving stereotactic radiosurgery. The other 13 recurrences were based on radiographic imaging.
Twelve of these patients had received prior external-beam radiosurgery with a mean dose range of 5,340 cGy to 6,400 cGy. Ten of the 19 patients had received chemotherapy as well.
A 9-year-old boy with pilocytic astrocytoma in the basal ganglia and a 60-year-old man with a low-grade oligodendroglioma in the thalamus/hypothalamus received definitive stereotactic radiosurgery.
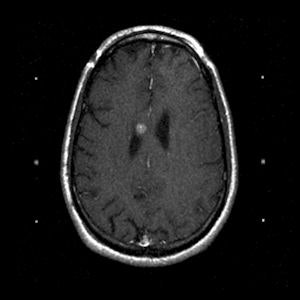 |
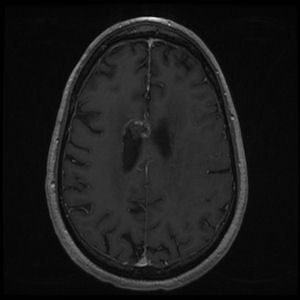
| A 43-year-old man with oligodendroglioma. Above, axial T1 + contrast brain MRI before Gamma Knife treatment. Below, axial T1 + contrast brain MRI two years after Gamma Knife treatment. Images courtesy of Dr. Allison Quick. |
 |
For all patients, a thin-cut (1.3- to 1.5-mm slices) stereotactic MRI exam was performed with axial T1 and T2 images used for planning. Gross tumor volume was contoured, and the single dose prescribed ranged from 1,000 cGy to 2,000 cGy prescribed to the 50% isodose line. The average dose was 1,611 cGy, and the average target volume was 6.34 cm³, with a range of 60.4 mm³ to 22.4 cm³.
The team defined the primary end point as local control, namely no radiographic evidence of tumor progression. Overall survival was the secondary end point, and the researchers used Kaplan-Meier analysis to calculate both, Quick said.
At the time of data collection, more than half of the patients had tumor progression, which on average occurred at 23.8 months, with a range of one month to four years. Seven patients were stable, and the tumors of two patients shrank. Local control rates were 77% at 12 months, 60.7% at 24 months, and 50.6% at 36 months. Because one patient died four years after treatment, overall survival was 83.3% at four years. The excellent overall survival was attributed to salvage therapies after recurrence, according to Quick.
"One thing to keep in mind when comparing our study to others reporting 50% to 70% local control at three years is that most of the patients in our study previously failed multimodality therapy," Quick said.
The researchers believe that their results are compatible with a study reported by Dr. C. G. Hadjipanayis and colleagues at the University of Pittsburgh's Center for Image-Guided Neurosurgery (Neurosurgical Focus, May 13, 2003, Vol. 14:5, pp. e5). These neurosurgeons reported a 67% local control rate in a cohort of 49 patients who received Gamma Knife stereotactic radiosurgery for recurrent or eloquently located pilocytic or grade II fibrillary astrocytomas. They found improved local control in the adjuvant group (24 patients) compared to the salvage cohort (25 patients), with rates of 71% and 64%, respectively.
The lower local control rate at two and three years in the study by Quick's team may be explained by the fact that 79% of the group's patients received treatment for recurrent disease, compared to 51% in the Hadjipanayis study.
"In our patient cohort, which we recognize was small in size, there was no significant difference between grade I and grade II gliomas," Quick said. "However, out of a group of four patients who were treated with a dose of 2,000 cGy, only one developed local progression, compared to nine who were treated with less than that amount."
Seven patients developed complications, five of whom had previously been treated with external-beam radiation. Three patients developed radiation necrosis, and one of these patients also had a seizure. One additional patient had a seizure, one patient had cystic progression, and two patients had severe symptoms from edema requiring steroids.
"Gamma Knife stereotactic radiosurgery is noninvasive with few complications," Quick concluded. "We believe it may be a means of stabilizing or delaying progression of disease for nonsurgical candidates. Higher doses seem to provide better local control, but may also increase the complication rate. For this reason, more studies are needed to address appropriate dose and effects on survival."
By Cynthia Keen
AuntMinnie.com staff writer
December 23, 2008
Related Reading
Stereotactic radiosurgery can extend survival in small recurrent glioblastomas, June 20, 2008
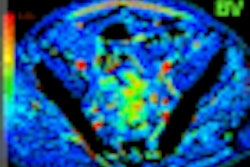
Perfusion MRI can predict progression of gliomas, April 30, 2008
Copyright © 2008 AuntMinnie.com