_p888_f1_thumb.png?auto=format%2Ccompress&q=70&w=400)
Eye cancer patients face an unenviable dilemma. They must enter treatment knowing that their surgeon's strategy to kill the deadly tumor with radiation may also sacrifice their eyesight: The odds are 50/50 that radiation damage to healthy tissue will negatively affect their visual acuity.
Now, a team of University of California, Los Angeles (UCLA) researchers has discovered that by applying a layer of silicone oil in the eye while radiation therapy is being administered, healthy tissue in the eye may be shielded and vision in patients undergoing treatment for uveal melanoma may be preserved.
So far, patients who have had the new surgical procedure have not experienced any vision loss, according to Tara McCannel MD, PhD, a vitreoretinal surgeon who also is director of the Ophthalmic Oncology Center at UCLA's Jules Stein Eye Institute and a member of UCLA's Jonsson Comprehensive Cancer Center.
While it takes six months to three years for a patient to develop increasing and irreversible vision loss, the first patient who underwent the procedure in February 2010 has reached the six-month mark with baseline visual acuity intact.
Rare cancers
Intraocular cancers are rare, with approximately 2,400 to 2,500 new cases diagnosed annually, according to 2010 cancer statistics from the American Cancer Society (ACS). Most ocular melanomas occur in the uveal tract, the vascular layer that includes the choroid (the pigmented layer under the retina), the ciliary body (the muscle that changes the size of the pupil and the shape of the lens when the eye focuses), and the iris.
The standard treatment for many patients is iodine-125 (I-125) brachytherapy delivered by an eye plaque. Many patients prefer this treatment to the alternative of enucleation, the surgical removal of the eye. However, during the days that the brachytherapy plaque is in place, healthy tissue in the eye is also irradiated.
Irreversible injury to the optic nerve fibers and macula, the portion of the retina responsible for central vision, may occur. Radiation damage to the macula weakens blood vessels feeding the eye, causing bleeds and wiping out circulation. Eye structures also become very fragile and prone to atrophy, which can also lead to vision loss.
This loss of visual acuity due to brachytherapy has been well documented by the Collaborative Ocular Melanoma Study (COMS), a set of multicenter clinical trials initiated in 1986 to evaluate the outcomes of patients with choroidal melanoma who either received I-125 brachytherapy treatment or enucleation. The study reported that visual acuity of patients during the first three years following radiation therapy declined at a rate of approximately two lines on a standard vision chart per year, on average.
Of the patients enrolled in COMS who received brachytherapy treatment, 43% to 49% had substantial impairment in visual acuity three years after treatment. The COMS research team defined this as a loss of six or more lines of visual acuity from pretreatment levels or a decrease from better than 20/200 at baseline to 10/100 or worse. At 30 months, 52% of 623 patients who received the radiation therapy treatment had visual acuity worse than 20/400.
Radiation attenuation
With these frightening statistics in mind, McCannel and Scott Oliver MD, then a vitreoretinal fellow who is now assistant professor of ophthalmology at the Rocky Mountain Lions Eye Institute of the University of Colorado in Aurora, brainstormed about the idea of testing different liquid vitreous substances commonly used in vitreoretinal surgical procedures to determine their radiation attenuation effect. They reported their research in an article published in the July 2010 issue of the Archives of Ophthalmology (Vol. 128, pp. 888-893).
In the laboratory, using eyes from cadavers, Oliver tested heavy oil, perfluorocarbon liquid, 5,000-centisoke silicone oil, and 1,000-centistoke silicone oil. He used a sodium chloride saline solution as a control.
The 1,000-centistoke silicone oil produced a 48% effect in attenuating radiation. Monte Carlo simulation of the human globe projected a dose reduction of 25% at the macula, 35% at the proximal optic nerve, 57% at the equator, and 58% at the ora serrata. Empirical data and theoretical calculations demonstrated that silicone oil attenuated radiation in the human eye by as much as 55% compared with saline.
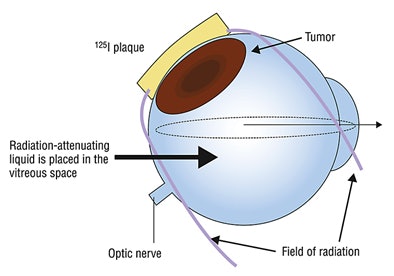 |
| Schematic drawing of vitreous substitution to shield vital intraocular structures during iodine-125 brachytherapy for uveal melanoma. Reprinted with permission from Archives of Ophthalmology, July 2010, Vol. 128:7, p. 889. Copyright © 2010 American Medical Association. All rights reserved. |
Clinical use
Oliver is continuing this research at the Rocky Mountain Lions Eye Institute, as a precursor for a formal clinical trial. McCannel, however, has moved ahead to apply the technique in the clinical realm.
In an interview with AuntMinnie.com, McCannel said that she initially had no intention of performing the procedure on any patients until the Archives of Ophthalmology paper was published. But when an engineer diagnosed with uveal melanoma was waiting for his scheduled plaque surgery, he discovered information about the research and a patent application on the UCLA website.
"The patient wanted to know why I had not offered this experimental surgical procedure to him, and after much discussion, he was adamant to be the first patient," McCannel said. "As an engineer, he understood the underlying physics, and he was very motivated. Neither he nor I felt that he had anything to lose. His surgery took place in February, and shortly after that our paper was accepted. I've continued to offer this procedure to patients who are good candidates, and who are also highly motivated to try unconventional treatment that might reduce the risk of losing their vision."
"I spend a lot of time discussing the procedure with potential candidates," she said. "When you do something additional in eye surgery, there may always be complications. So far, none of the patients have experienced any loss of visual acuity and there have been no complications. However, it is too soon to determine just how successful this will be in the long term. The six-month, one-year, two-year, and three-year outcomes will be critical determinants."
The surgical procedure
Surgeons at UCLA use an eye plaque consisting of a custom-fabricated gold shield onto which spherically symmetric brachytherapy I-125 seeds are glued onto the inner surface. The plaque opening is then filled with a tissue-equivalent sealant material, McCannel explained.
The surgery begins with plaque placement. A fine-needle aspiration biopsy is performed to determine the tumor's monosomy 3 status -- the risk factor most strongly associated with metastasis. Intraoperative ultrasound is performed to confirm the accurate position of the plaque before permanent suturing.
McCannel then performs a complete pars plana vitrectomy that removes the entire vitreous gel. It is performed using microsurgical instruments introduced to the back of the eye, with an operating microscope and wide-angled viewing of the retinal fundus. Once all the vitreous is removed, the eye is filled with 1,000-centistoke silicone oil (Silikon 1000, Alcon Laboratories, Fort Worth, TX), and the incisions are sutured closed.
The patient keeps the plaque and the oil in the eye for several days until the calculated dose of radiation to the tumor is released. The silicone oil does not affect the calculated radiation dosing, McCannel explained, and during this time, the patient can see almost as well as before the surgical procedure.
The plaque is removed in the usual manner, the silicone oil is aspirated, and saline is used to fill the eye. With the suturing of the incision in the eye, the treatment is finished.
Patients who have this procedure probably will develop cataracts, although this hasn't happened yet. "Cataracts, detached retinas -- these conditions an ophthalmologist can fix," McCannel said. "What nobody is able to correct is vision loss from radiation damage. Once it happens, it is permanent. We are all very hopeful that the silicone oil will prove to be as effective as a protective shield to healthy tissues as it proved to be in rigorous laboratory tests."
By Cynthia E. Keen
AuntMinnie.com staff writer
August 16, 2010
Related Reading
New technology spurs investment in brachytherapy, April 23, 2009
Cancer drug curbs radiation-induced vision loss, July 9, 2007
Radiotherapy may preserve eyes with large uveal melanomas, June 21, 2006
High-dose strontium-90 brachytherapy effective for posterior uveal melanoma, October 31, 2005
Copyright © 2010 AuntMinnie.com