The adoption of intensity-modulated radiation therapy (IMRT) has prompted sharply higher costs for radiation therapy, according to an April 29 article in the Journal of the National Cancer Institute. The study found that it cost twice as much to use IMRT to treat women with breast cancer compared with traditional radiation therapy.
The study, led by Dr. Benjamin D. Smith, assistant professor in the department of radiation oncology at MD Anderson Cancer Center, reviewed Medicare data for 26,163 women ages 66 years and older with localized breast cancer who had undergone surgery and radiation therapy from 2001 to 2005.
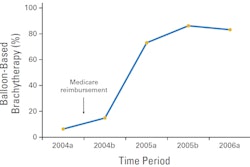
Smith and colleagues found that Medicare billing for IMRT increased more than 10-fold, from 0.9% (49 of 5,196) of patients diagnosed in 2001 to 11.2% (564 of 5,020) of patients diagnosed in 2005.
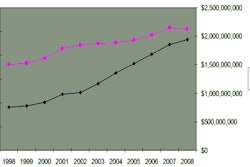
The average cost of radiation within the first year of diagnosis was $7,179 without IMRT and $15,230 with IMRT. In addition, the mean total cost of all healthcare within the first year of diagnosis was $21,674 for non-IMRT patients, compared with $29,366 for IMRT patients. In other words, within the first year of diagnosis, radiation therapy-related costs accounted for 33% of total medical care costs for non-IMRT patients and 52% of total medical care costs for IMRT patients.
In addition, the researchers found that the mean radiation therapy-related costs within the first year of diagnosis were 28% greater ($9,451 versus $7,391) for patients residing in regions with favorable Medicare reimbursement for breast IMRT, compared with patients in regions with less favorable payments for breast IMRT.
IMRT billing was also more frequent for patients treated by radiation oncologists in freestanding radiation oncology centers (7.6% had IMRT), compared with patients treated in hospital-based outpatient clinics (5.4% had IMRT).
The authors noted two ways to achieve intensity modulation of the radiation beam, one called field-in-field forward planning and one called inverse planning. The second option is more expensive, requiring more physician and treatment planning time. Most Medicare carriers require inverse planning to reimburse for IMRT, although the two approaches likely have similar outcomes in cases in which only treatment of the breast is necessary, the authors wrote.
The data "suggest that with respect to breast radiation therapy, much of the variation in cost can be directly attributed to inconsistent treatment definitions and reimbursement rates authorized by Medicare and its intermediaries," Smith and colleagues concluded.