Are randomized clinical trials appropriate for demonstrating proton therapy's superiority to x-ray therapy? The European Society for Therapeutic Radiology and Oncology (ESTRO) meeting, held last month in London, was the venue of a contentious debate on this subject.
"We do not need randomized clinical trials to demonstrate that proton therapy is superior to x-ray therapy," said Dr. Hideyuki Sakurai, PhD, director of the University of Tsukuba's Proton Medical Research Center (PMRC) in Japan, a research institute that has performed approximately 3,000 proton-beam treatments to date. Sakurai is firmly convinced that there is no need for randomized trials of proton versus photon therapy.
"We are conducting six phase II trials at PMRC, but there are no randomized phase III trials in our institute," he said, before listing a number of reasons as to why this is the case.
First up: the ethical considerations. Can the patient accept the results of a coin flip? Sakurai explained that the two arms in a randomized trial need to be substantially equivalent from the patient's view. But while biological processes are fraught with uncertainty, physics is different, he said, explaining that protons are known to deliver less dose to normal tissue than photons.
"This is the first doubt for comparing protons versus x-rays," he said. "The physics is well-known before the clinical trials."
Other issues to consider include cost, lack of resources (few particle therapy centers per population), and time requirements for randomized trials. For example, health insurance in Japan covers radiotherapy but not particle therapy. So who pays the treatment fees for the patients randomized to receive protons? For rapid progression of proton therapy, Sakurai proposes nonrandomized phase I and II studies instead.
Sakurai then discussed the appropriateness of randomized clinical trials for some specific disease examples. For pediatric cancers, the case is pretty much closed. With the absolute indications for proton therapy in such cases, randomized comparisons with photon radiotherapy are not just unnecessary, but unethical, he told the ESTRO delegates.
Likewise, for hepatocellular carcinoma (HCC), physics studies suggest that proton therapy can save more liver function than photon radiotherapy. Sakurai proposed that randomized trials for HCC should examine proton therapy versus radiofrequency ablation (for small tumors) or surgery (for large tumors), but not compare photons with protons.
In some cases, such as localized prostate cancer and early-stage lung cancer, there are no clear advantages of proton therapy over advanced radiotherapy modalities. Intensity-modulated radiotherapy (IMRT) offers high local control and a low incidence of side effects for treating localized prostate cancer, while stereotactic body radiation therapy (SBRT) offers similar performance for early-stage lung cancer.
Sakurai noted that one would expect good results from both arms in randomized trials for these diseases. Such trials could really only prove that expensive proton therapy is noninferior to lower-cost x-ray treatments.
Sakurai concluded by noting that with increasing physics-based (dosimetric) evidence of proton therapy's superiority, and increasing clinical evidence from nonrandomized studies, the fact that there's no evidence from randomized trials is not a reason for denial.
"Ongoing studies with more patients and longer follow-up will demonstrate the true indications of particle therapy," he said.
The burden of proof
Refuting Sakurai's argument, Dr. W. Robert Lee, a radiation oncologist at Duke University Medical Center in Durham, NC, told the assembled audience that within science the burden of proof always lies with the claimants.
"The claim is that proton therapy is superior to photon therapy. If proton advocates believe this to be the case, then they must prove it by accumulating evidence," he said.
"Evidence" comes in many forms: from intuitive to that gained via personal experience to anecdotal. "But what's really needed," Lee said, "is scientific evidence that's hypothesis-based, empirical, reproducible, and falsifiable. It's accepted that randomized clinical trials are the best way to provide such evidence."
Without such rigorous trials, Lee suggested, results can be subject to confirmation bias, the tendency for people to favor information that confirms their preconceptions or hypotheses, regardless of whether the information is true.
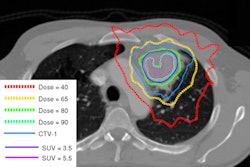
Lee pointed out that while the physics of protons may indeed be predictable, the actual delivery of proton therapy comes with many uncertainties. These include CT approximations, tissue inhomogeneities, and uncertainties in acceleration energy, scattering systems, and compensator density.
Thus the actual location of the distal margin on any given day is uncertain and so one must be highly cautious about the use of dose-volume histograms to argue for superiority. Clinical results in patients are more meaningful. But there is a complete lack of evidence from randomized trials comparing protons and photons, he pointed out.
"Statements about superiority in any realm of clinical medicine in the absence of randomized clinical trials should be viewed with suspicion," Lee concluded. "To aver that protons are superior in the absence of randomized clinical trials isn't evidence-based medicine. It's faith-based medicine."
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.