Use of stereotactic body radiation therapy (SBRT) in the U.S. is escalating rapidly, according to survey findings described this month in Cancer and in three poster presentations at last week's American Society for Radiation Oncologists (ASTRO) annual meeting.
SBRT began to be used for cancer treatment in the early 1990s, with pioneering research conducted at Karolinska Hospital in Sweden. Growing use of SBRT technology in Japan was stimulated by Japanese governmental health insurance approval in 2004. Now, utilization of the technology in the U.S. has taken off as well, according to a survey of ASTRO members by researchers from the University of California, San Diego (UCSD).
Use of SBRT has increased by approximately 600% between 2004 and July 2010, if survey responses are representative. The treatment is primarily used for lung, spine, and liver cancers (Cancer, October 1, 2011, Vol. 117:19, pp. 4566-4572).
Researchers at UCSD's Center for Advanced Radiotherapy Technologies polled 1,600 randomly selected ASTRO members with a 21-question survey in 2010. They received 510 evaluable responses from radiation oncologists working in 48 states and the District of Columbia. The majority of respondents were in private practice (62.5%), with a median of 16 years of practice.
Nearly two-thirds of respondents were using SBRT equipment, and approximately half had acquired the technology in 2008 or later. Three-fourths were planning to increase their use. Of the 36% who weren't yet offering SBRT, the majority planned to do so in the near future.
The most commonly treated cancers were lung (51.8%), spine (39%), and liver (31%). Lead author Hubert Pan, a third-year medical student at UCSD, and colleagues discussed the survey findings regarding treatment for these three cancers in poster presentations at the ASTRO meeting.
Lung
Lung cancer was the most common disease treated with SBRT, cited by 275 (64%) of the respondents. Younger radiation oncologists who had been practicing fewer than 10 years were more likely to use the technology, as were radiation oncologists working at academic cancer treatment centers. As might be expected, radiation oncologists specializing in lung treatment were more likely to use SBRT, at 81% compared to 50%, Pan said.
The three most commonly prescribed treatment regimes were three fractions at 20 Gy (22%) or 18 Gy (21%), and four fractions at 12 Gy (17%). Unsurprisingly, the three-fraction dose of 20 Gy replicated the dose used in the Radiation Therapy Oncology Group (RTOG) 0236 clinical trial, which evaluated the use of SBRT for medically inoperable patients with early-stage non-small cell lung cancer (NSCLC). Respondents were more likely to deliver treatment in three fractions if they used fiducial markers (31% of the total), used 2D planar imaging for target localization, or were early adopters of the technology.
The median biological equivalent dose (BED) was 132 Gy. All but 5% stated that a BED greater than 100 Gy was administered. Respiratory-induced motion was managed by abdominal compression using a stereotactic body frame and by respiratory gating. Breath-hold techniques were infrequently used.
The researchers noted that with increasing adoption of in-room volumetric imaging, a future study may identify a decline in the use of fiducial markers.
Spine
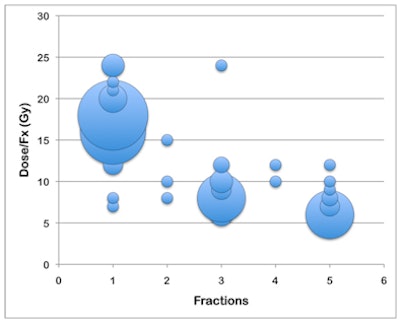
The same number of respondents also used SBRT to treat cancerous tumors in the spine, although with less frequency. The majority (57%) administered the radiation dose in one treatment, with the most common prescriptions being either 18 Gy or 16 Gy. Single-fraction treatments were constrained by maximum spinal cord doses of less than 14 Gy by 91% of respondents and less than 10 Gy by 61%. The RTOG guideline for spinal cord dose tolerance is not to exceed 14 Gy, and this guideline was followed by almost all radiation oncologists.
One trend identified by the researchers was that prescribing a single SBRT treatment for spine tumors was more prevalent in large practices having more than seven radiation oncologists, and by radiation oncologists who treated larger numbers of these patients.
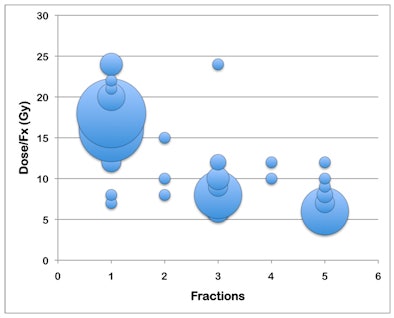 |
| Bubble chart of the most common spine SBRT prescriptions. The size of the bubble corresponds to the number of responses. The largest bubbles reflect prescriptions of 18 Gy x 1 (22%), 16 Gy x 1 (20%), 8 Gy x 3 (11%), and 6 Gy x 5 (11%). Image courtesy of the Department of Radiation Oncology, Center for Advanced Radiotherapy Technologies, UCSD. |
Liver
Slightly more than half of the respondents used SBRT to treat liver cancer. Treatment was administered in three to five fractions, with three fractions of 15 Gy being the most commonly reported regime. The median BED was 106 Gy; 12% treated patients with a BED of 180 Gy, administered in three fractions of 20 Gy.
Fiducial markers were used by 57% of respondents. More than half of the radiation oncologists managed respiratory-induced motion by using respiratory gating or abdominal compression. Stereotactic body frames tended to be used more often when a higher BED was prescribed.
Pan said that he believes this 2010 survey was the first of its kind to investigate the use of SBRT technology in-depth in the U.S. "With such rapid technological innovations happening in the field of radiation therapy, it's interesting to see how quickly the ASTRO community adopts them," he said.