Radiation therapists are responsible for the safety of patients who are undergoing radiotherapy treatments. Do they know if their safety standards and responsibilities correspond to best-practice guidelines and recommendations?
Addressing this question is the goal of a new white paper issued this week by the American Society of Radiologic Technologists (ASRT) that defines the roles and safety responsibilities of radiation therapists. Developed by a subcommittee of the ASRT Education and Research Foundation's Health Care Industry Advisory Council, it highlights best practices and recommendations focused on workplace staffing, workplace culture, skills assessment, and applications training and support.
The paper was developed in part as a response to a series of articles published in the New York Times about serious errors made during radiation therapy treatments. The series also describes regulatory oversight gaps and inconsistencies by federal and state agencies.
Need for more collaboration
The white paper materialized from a discussion about the need for more collaboration between facilities and vendors with respect to training radiation technologists about new equipment and new technology, Liana Watson, ASRT's chief governance and development officer, told AuntMinnie.com.
The discussion took place during the ASRT foundation's Health Care Industry Advisory Council summit held in May 2011. The summit brings together companies in the radiation therapy and medical imaging industry to work together in a noncompetitive environment to advance patient care.
The summit participants created the subcommittee at the meeting, which included radiation therapy managers, representatives from radiation therapy equipment manufacturers, and representatives from the ASRT board of directors and the American Registry of Radiologic Technologists board of trustees. The subcommittee then met at ASRT headquarters in Albuquerque, NM, in November 2011 to develop the paper.
Recommendations
There should be a minimum of two ASRT-registered radiation therapists for each treatment machine, with one of the therapists focused on the patient and the other on the treatment console. An additional two therapists should be available in the event of emergencies and to verify information during time-outs for procedures. Treatment facilities need to review staffing schedules to determine if there is any time when this requirement is not met and make appropriate changes.
Every radiation oncology department should establish a workplace culture that strongly mandates reporting of clinical errors and near misses. Radiation therapists should be required to document all errors and exceptions that deviate from well-defined, well-established criteria and procedures.
They should participate in continuous process-improvement activities and be involved in patient-safety committees. A department should schedule a radiation therapist's time to include these activities.
Procedural checklists should be routinely used. Routine double-checking should also be incorporated within a radiation oncology department of any size, with time scheduled for radiation therapists to perform this activity, as well as perform time-out checks. Efforts should be made to minimize distractions by discouraging staff from interrupting therapists. Workstations should be uncrowded, with all activities focused on the job at hand.
In view of the continuous software upgrades, technology innovations, and protocol changes relating to radiotherapy treatment, frequent and regularly scheduled skills assessment of radiation therapists needs to be performed by a radiation oncology department or treatment center. For each type of treatment procedure, checklists should be developed that represent the core competencies a radiation therapist must have to perform treatment. Therapists who have knowledge deficiencies should be given the time and the training to rectify them.
Peer review and assessment is also recommended. This can include chart checks to verify that standard operating procedures are being followed. Deviations from standard operating procedures need to be investigated, and if they're not justified, they need to be managed in the context of quality-assurance improvement rather than through punitive means.
The ASRT white paper recommends that whenever new equipment is being installed, radiation therapists must be prepared with the basic knowledge required to work on the new modality prior to installation. If radiation therapists do not understand the basics of the technology and modality prior to the vendor's applications training, they risk not thoroughly learning what they are taught.
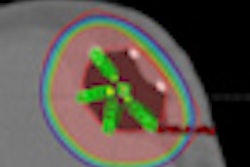
The paper uses the example of adding intensity-modulated radiotherapy (IMRT) capability to a radiation oncology practice. In addition to taking courses in advance, radiation therapists also should be thoroughly trained in CT simulation. Ideally, radiation therapists will have CT certification.
Radiation therapists should also be willing to take unscheduled quizzes that will confirm their competency. These also should be administered to new and temporary staff.
The importance of application training
Members of the ASRT subcommittee who work as clinical applications trainers for vendors were especially vocal about the need for providers to be thoroughly prepared for scheduled training. Shortcutting applications training is not an option for providers, the paper emphasized.
Customers installing and updating equipment must regard uninterrupted applications training as a requirement for all staff rather than an option and schedule accordingly. One of the problems that applications trainers say they frequently encounter is that during scheduled sessions, radiation therapists are interrupted to perform department work. This is not acceptable, the report states.
Radiation therapists should have successfully completed any advance coursework or training prior to the company applications training sessions. Even the best-planned training session can be undermined if a participant isn't up-to-speed with respect to assumed baseline knowledge.
Customers should demand that applications training include problem-related scenarios requiring troubleshooting and error correction. Radiation therapists should have a sound understanding of how to resolve the most common equipment-performance problems to minimize help-desk calls.
Applications training should be scheduled for new staff when needed.
Vendors, sites, and staff share ownership and accountability in facilitating successful training, the ASRT subcommittee emphasized. As an outcome from developing the paper, the subcommittee stated it will spearhead efforts to provide guidelines for successful radiation therapy equipment installation and training. These will include preparedness and competency checklist suggestions.
Expectations
"We hope that this white paper will have widespread dissemination and have a positive impact on clinical practice," Watson said. "Providing radiation therapists and applications trainers with best practices and recommendations that they can bring to the workplace and discuss with their coworkers and managers was a key strategy of the subcommittee."
ASRT hopes that by providing therapists and equipment applications trainers with concrete tactics that can be implemented with the support of the department will be very beneficial to all parties and ultimately to the safety of patients.
The white paper is already on the agenda of the May 2012 summit. Watson said that attendees will discuss how the paper is being used and what impact it is having.
A downloadable copy of the white paper may be accessed here.