The combination of chemotherapy and concurrent radiation therapy (RT) lengthened survival for elderly patients with unresectable stage III non-small cell lung cancer (NSCLC), according to a report by Japanese researchers published online May 22 in Lancet Oncology.
However, the majority of patients who received chemoradiotherapy had toxicities that none of the radiotherapy-only patient group experienced, and more than twice as many had grade 3 infections. Treatment-related deaths were comparable for the treatment groups.
The findings of this randomized phase III trial by the Japan Clinical Oncology Group help clarify whether chemoradiotherapy, the standard treatment for patients with locally advanced NSCLC, is suitable for patients older than 70. More than two-thirds of lung cancer cases occur in people 65 years of age or older.
The objective of the clinical trial was to determine whether radiotherapy alone or chemotherapy with radiation therapy improved survival. The researchers also sought to compare response rates to treatment, progression-free survival, sites of progression, and toxicity.
Between September 2003 and May 2010, 200 patients being treated at 27 hospitals were enrolled in the trial and evenly randomized to each group. The median age for each group was 77, with men representing at least 80% of each group. Disease stage, tumor stage, nodal involvement, amount of weight loss, smoking history, and comorbidities were comparable between the groups.
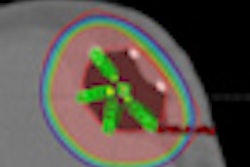
Patients in the chemoradiotherapy group received daily low-dose carboplatin one hour before their radiotherapy treatments for the first 20 fractions. All patients received a radiation dose of 60 Gy, consisting of 40 Gy delivered in 30 fractions over six weeks plus a boost dose of 20 Gy to the primary tumor and metastatic lymph nodes.
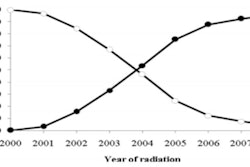
Results showed that patients given the chemoradiotherapy treatment were nearly a third less likely to die at a median follow-up of 19.4 months, according to principal investigator Dr. Shinji Atagi, a radiation oncologist at Kinki-Chuo Chest Medical Center in Osaka, and co-authors. The median overall survival for the chemoradiotherapy group was 22.4 months, compared with 16.9 months for the radiotherapy-only group.
A total of 88 patients completed the chemoradiotherapy treatment and 93 patients completed the radiotherapy-only treatment. One year after treatment, 70.8% in the chemoradiotherapy group were alive, compared with 46.3% of the radiotherapy-only group. Survival outcomes were equally impressive two years following treatment, at 65.2% and 35.1%, respectively.
Median progression-free survival was also better for the chemoradiotherapy group, at 8.9 months with the combined treatment, compared with 6.8 months in the radiotherapy-only group.
However, the chemoradiotherapy group experienced a much higher rate of grade 3 and 4 toxicities. Almost two-thirds of the patients experienced leukopenia, 57% had neutropenia, and 30% had thrombocytopenia. By comparison, no patients in the radiotherapy-only group had grade 3 or 4 leukopenia or neutropenia, and only two had thrombocytopenia.
Grade 3 infection was three times higher in the chemoradiotherapy group (12.5% compared to 4.1%). Nearly twice as many patients receiving the combined therapy experienced fatigue.
The researchers did not assess how these toxicities affected the quality of life that remained for each group of patients.
In a published comment, Dr. Juan Wisnivesky, PhD, a pulmonologist and epidemiologist at Mount Sinai School of Medicine, and Dr. Gary Strauss, medical director of the lung cancer program at Tufts Medical Center, cautioned that while the outcomes of the study are positive for the combined treatment, broader validation of the findings should be conducted in clinical trials with a broader population of older patients more equally matched by gender.