When a patient with organ-confined prostate cancer needs radiation therapy, replacing intensity-modulated radiation therapy (IMRT) with stereotactic body radiation therapy (SBRT) may be more cost-effective, according to an article published in the May issue of the Journal of Oncology Practice.
A model developed by researchers at the University of Texas Southwestern in Dallas to evaluate the cost-effectiveness of the two external-beam radiation treatment options suggests that use of SBRT in lieu of IMRT for just half of the patients who need the treatment could potentially save $250 million annually (J Oncol Pract, Vol. 8:3S, pp. e31s-e37s).
The American Cancer Society estimates that in 2012, 242,000 men living in the U.S. will be diagnosed with prostate cancer, and approximately 41% will be diagnosed with organ-confined prostate cancer. In 2010, the cost to treat prostate cancer patients was more than $12 billion, making this disease the fifth most costly cancer to treat in the U.S., according to the National Institutes of Health.
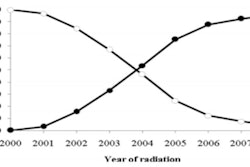
Over the past decade, IMRT has replaced 3D conformal radiation therapy as the treatment of choice for the 35% to 46% of patients with organ-confined prostate cancer who elect to undergo radiation therapy. Starting as early as 2000, but more recently within the past five years, some patients enrolled in clinical trials received SBRT. To date, reports of early outcomes have been comparable to IMRT-treated patients.
Because SBRT delivers a higher dose of radiation per fraction, there are fewer treatments; this reduces disruption for patients and potentially lowers the cost of treatment-related expenses. In fact, a Radiation Therapy Oncology Group (RTOG) trial still enrolling patients is comparing a five-fraction SBRT course with a 12-fraction IMRT course, with a primary end point of patient-reported quality of life a year after treatment.
Lead author Dr. Joseph Hodges and colleagues developed a Markov decision-analysis model that incorporates sensitivity analysis to evaluate the cost-effectiveness of the treatments, based on a 70-year-old patient with various disease states who would be followed for up to 10 years.
Defining the factors that comprise cost-effectiveness as cost, efficacy, and quality of life, the authors calculated that patients treated with either modality had a mean quality-adjusted life year score of 7.9. However, the mean cost of treatment for SBRT was $22,152, compared with $35,431 for IMRT.
More widespread adoption of SBRT for this type of prostate cancer patient could have a profound economic impact from both societal and individual patient perspectives, the group concluded.
They recommended that future studies evaluating SBRT focus on both acute and long-term quality-of-life outcomes, as well as efficacy. Quality-of-life outcomes affect all patients, whereas differences in the risk of cancer recurrence affect only a small percentage of patients.
"A 5% decrease in quality of life for one treatment results in an absolute decrease in quality of life of 5%," they wrote. "On the other hand, a 50% increase in recurrence only affects an additional 1% of patients, from 2% [of the total] to 3%."