Large-breasted women pose a challenge when radiation therapy (RT) for early-stage breast cancer is being planned and performed. Using a bra or bustier improves simulation and positioning in the supine position, according to an article published in the January issue of Practical Radiation Oncology.
Conventional tangential whole-breast radiation is often associated with greater than 10% dose heterogeneity across the target volume of a large breast. Because large pendulous breasts may displace laterally, a patient may experience larger chest wall separation when positioned in a supine position. This can increase the incidental dose delivered to the lung and heart, and for this reason, treatment in a prone position is often recommended, wrote lead author Lanea Keller, from Fox Chase Cancer Center, and colleagues (Pract Radiat Oncol, January 2013, Vol.3:1, pp. 9-15).
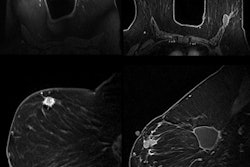
Radiation oncologists at Fox Chase Cancer Center have been using commercially available bras or corsets for simulation and treatment for some large-breasted patients. Keller and colleagues conducted a retrospective study to gather data on how a bra affects acute toxicity and dosimetry, including chest wall separation and lung and heart dose.
The patient group consisted of 246 women with a bra size of at least 38 and a cup size of C to EEE who were treated for early-stage breast cancer from 2001 through 2006. Of the group, 58 women wore a bra during treatment and 188 did not. Patients for whom a bra/bustier was recommended were custom-fitted based on chest and cup size.
All patients were treated with whole-breast radiation, either 3D conventional radiation or intensity-modulated radiation therapy (IMRT), in daily fractions of 2 Gy to a median dose of 46 Gy. Total dose was determined by the extent of surgery and final margins and ranged from 60 Gy to 66 Gy. Patients also received a boost dose with the bra removed.
The researchers compared dosimetry with and without a bra in a subgroup of 12 patients. The use of a bra was associated with 63.4% less heart volume in the treatment field, according to the group. Chest wall separation also decreased, and the amount of left lung in the treatment field was reduced by 19%.
Use of a bra allowed repositioning of the breast in the supine position, which significantly reduced the chest wall separation and, thus, resulted in a smaller volume of heart present within the treatment field, Keller and colleagues wrote.
However, the patients who wore bras/bustiers had more skin toxicities: 90% had grade 2 toxicities and 5.2% had grade 3 toxicities. By comparison, 70% of the group treated without a bra experienced grade 2 toxicities and 2.1% had grade 3 toxicities. For both groups, IMRT use was associated with reduced grade 2/3 skin toxicity (from 91% with conventional treatment to 68% with IMRT).
The patients are being followed to monitor long-term cosmetic outcomes.