MRI and CT are imaging's gold standards for patients with suspected pancreatic disease, but both are costlier and more time-consuming than ultrasound. So researchers from Philadelphia decided to test sonography's mettle, both pre-and post-contrast. Using CT and MRI data to corroborate the results, they found ultrasound to be highly effective in imaging pancreatic pathology -- and even more so when oral contrast was used.
 |
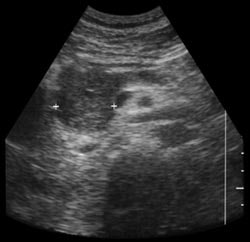 |
| Shadowing from bowel gas prevents visualization of pancreatic carcinoma (left). Following administration of SonoRx, a large hypoechoic mass is seen in the head of the pancreas (right). Images courtesy of Bracco Diagnostics. | |
Dr. Anna Lev-Toaff of the Thomas Jefferson University Hospital presented early results of the study at the abdominal scientific sessions of the American Institute of Ultrasound in Medicine conference in April.
Twenty-five patients with suspected pancreatic pathology underwent ultrasonography before and after ingesting 400 ml of SonoRx, a simethicone-coated cellulose oral contrast agent manufactured by Bracco Diagnostics of Princeton, NJ. The agent works by absorbing and dispersing gas bubbles in the stomach, thus reducing shadow artifacts.
"(SonoRx) creates a more uniform interluminal echogenicity, and allows for delineation of the normal gastric wall, and in many cases even the discrete layers," Lev-Toaff said.
The sonographer and interpreting radiologist were blinded to the CT and MRI results. The readers scored pre-and post-contrast sonograms of the pancreatic head, body, and tail visualization and diagnostic confidence on a scale of 1-5. In addition, each pancreatic segment was judged normal or abnormal with a confidence level of 1-5.
"We found that the sonographic visualization of the pancreas was improved after contrast, as was the diagnostic confidence," Lev-Toaff said. While scores rose in every category, the most dramatic improvements were seen in the pancreatic tail, where visualization increased from 2.0 to 3.8, and diagnostic confidence rose from 2.3 to 3.8. T-tests of the findings were also significant (p<.001) for the head, body, and tail, and sensitivity was greater post-contrast (100%) than pre-contrast (78%). Specificity remained unchanged at 88%.
Head and tail lesions that were missed pre-contrast were identified post-contrast in three patients. In addition, two nondiagnostic cases became diagnostic post-contrast, and lesions were identified post-contrast in two patients with indeterminate pre-contrast diagnoses, Lev-Toaff said. The study will continue until 50 patients have been examined.
One audience member sought guidance on when to use the agent, since "it represents a non-reimbursable expense." Lev-Toaff said that pending the addition of a new billing code, one approach was to do the ultrasound without contrast to see if the findings match the clinical suspicion. If there's no match, it makes sense to do a second procedure with contrast, she said.
Panel moderator Ana Monteagudo of New York University asked if there were any "special tricks" to administering the agent for optimal value. Lev-Toaff said patients need to be positioned in very specific ways to get the contrast to the area being studied. "It does require some creativity on the part of the examiner," she said.
By Eric Barnes
AuntMinnie.com staff writer
May 2000
Related Reading
"Ultrasound of the hepatobiliary-pancreatic system," World J Surg 2000 Feb;24(2):166-70
"Preoperative staging of pancreatic adenocarcinoma: a practice survey of French gastroenterologists and digestive surgeons. Ordering of supplemental examinations and preoperative criteria of loco-regional spread," Gastroenterol Clin Biol 1999 Oct;23(10):1055-61.
"Role of EUS in the preoperative staging of pancreatic cancer: a large single-center experience," Gastrointest Endosc 1999 Dec;50(6):786-91
Let AuntMinnie.com know what you think about this story.
Copyright © 2000 AuntMinnie.com


















