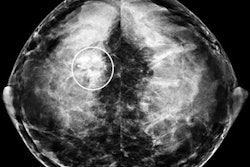
When high-quality equipment is paired with meticulous attention to scanning details, breast ultrasound yields increasingly definitive diagnostic information.
By applying a strict algorithm for differentiating benign from malignant lesions, sonographers can make more specific diagnoses, prevent biopsy of benign lesions, and find palpable malignant tumors missed by mammography, said Dr. A. Thomas Stavros, chief of ultrasound at Radiology Imaging Associates in Greenwood Village, CO.
Moreover, such findings can be correlated with the Breast Imaging Reporting and Data System (BI-RADS) developed for mammography by the American College of Radiology.
Stavros reviewed breast ultrasound techniques for both diagnosis and staging at the 2003 National Consortium of Breast Centers meeting in Las Vegas.
Assessing palpable abnormalities and evaluating mammographic irregularities are the key indicators for breast ultrasound. Stavros has a long track record of studying the viability of ultrasound to reliably distinguish benign from malignant nodules (Radiology, July 1995, Vol. 196:1, pp. 123-134).
Based on as-yet-unpublished work, Stavros reported achieving better than 98% sensitivity with ultrasound when adhering to a strict algorithm, one that demands identification of multiple characteristics of malignant or benign lesions.
"Breast cancer is too heterogeneous to be solved by a single finding," Stavros said. "The average cancer that we see has five or six positive findings. Even if we are having a bad day, even if we missed four, we are still going to find one or two others."
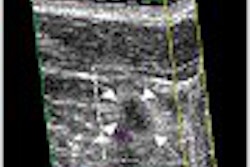
Malignant lesions can present with several characteristics on ultrasound:
- Spiculation.
- Taller-than-wide (larger AP than transverse dimensions).
- Angular margins.
- Markedly hypoechoic (compared to fat).
- Shadowing.
- Calcifications.
- Duct extension.
- Branch pattern.
- Microlobulation.
Care needs to be taken with all solid nodules. Malignant findings should be sought and their presence or absence recorded. If even a single malignant feature is present, the nodule cannot be classified as benign.
Of the nine key findings, some carry more weight than others. Spiculation, angular margins, and acoustic shadowing are "hard" findings most commonly found in conjunction with invasive disease, he said.
Duct extension, branch pattern, and calcifications are considered soft findings. Microlobulation can be either a hard or soft finding, he said. Hypoechogenicity and taller-than-wide, when seen in the absence of other findings, are considered nonspecific.
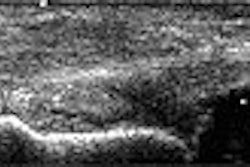
If no malignant features are found, specific benign features need to be sought. These include:
- Absence of any malignant findings.
- Markedly hyperechoic (compared to fat).
- Ellipsoid shape.
- Three or fewer lobulations.
- Thin, echogenic capsule.
A nodule can be classified as benign only if benign findings are found, he said. If specific benign features are not found, the lesion should be classified, by default, as indeterminate.
But in Stavros’ experience, regardless of lesion size, if no suspicious features exist and one of three benign features are present, "We can be fairly certain that we are dealing with a less than 2% chance of cancer," he said.
BI-RADS correlation
In mammography, patients are categorized as BI-RADS 3 if their cancer risk is 2% or less. At the NCBC meeting, Stavros presented a modified version of BI-RADS for use as a guidepost by sonographers. The ACR has not sanctioned BI-RADS for use with either ultrasound or MRI.
| Ultrasound BI-RADS Chart Breast imaging reporting and data system |
||
 |
||
| Risk of cancer | Description | |
 |
||
| Category 1 | negative | negative |
 |
||
| Category 2 | 0% | benign |
 |
||
| Category 3 | less than 2% | probably benign |
 |
||
| Category 4a | 3-49% | mildly suspicious |
 |
||
| Category 4b | 50-89% | moderately suspicious |
 |
||
| Category 5 | 90% or greater | malignant |
 |
||
| Developed by Dr. A. Thomas Stavros; presented at 2003 NCBC. | ||
"It’s not a wild and crazy scheme, it’s the mammographic algorithm applied to ultrasound with a few extra steps," Stavros said. "And there’s a solid morphologic basis for our findings. We can identify a BI-RADS 3 group that has a less than 2% chance of cancer with a negative predictive value that is greater than 98%."
Stavros divides the mammographic BI-RADS 4 into two categories for ultrasound. BI-RADS 4a includes patients whose cancer risk is between 3%-49% based on sonographic findings. BI-RADS 4b includes patients whose risk falls between 50% and 89%. BI-RADS 5 includes patients in the 90% and above risk category.
"We divided BI-RADS 4 at the 50% line, because 50% is the medical-legal definition of probable," he said. "To have any system that doesn’t take into account medical-legal definitions as probable is probably flawed."
At the NCBC meeting, Stavros emphasized the importance of careful scanning of patients who potentially fall into the BI-RADS 3 category, which is significant because it carries a 97% chance that the lesion is not cancer.
At Radiology Imaging Associates, patients with solid nodules are scanned by Stavros personally. Those classified as BI-RADS 3 are counseled as to their options: surgical incision, an ultrasound-guided biopsy, or short-term follow-up.
"I tell BI-RADS 3 patients that nothing is 100%, but I’m pretty good at this and I’m more than 98% sure that their lump is benign. About 40% of patients want to be biopsied and about 60% are willing to be followed," he said. "I think it all depends on how you talk to them."
While there has been discussion in the mammography community about suspending the six-month follow-up for BI-RADS 3 patients, Stavros thinks doing so would be a mistake for ultrasound practitioners.
"Our misses are going to be on the circumscribed end of the spectrum, and what lives there is high-grade invasive ductal cancer," he said. "(Such tumors) grow fast and change rapidly. I’m very uncomfortable with the concept of giving up six-month follow-up in these patients."
By Deborah R. DakinsAuntMinnie.com contributing writer
April 17, 2003
Related Reading
Contrast-enhanced 3-D US boosts mammography results, April 11, 2003
New adjunctive breast techniques improve positive biopsy rates, February 25, 2003
Mammo plus US negates need for breast MR, December 23, 2002
Copyright © 2003 AuntMinnie.com