Around the world, contrast-enhanced ultrasound is available for a myriad of radiological applications. In the U.S., however, the Food and Drug Administration has cleared its use only for imaging the left ventricle of the heart, and this huge disparity in allowed applications clearly has some U.S. practitioners frustrated.
"The FDA has refused to approve any contrast agent for anything but the most trivial applications in echocardiography. I think we can safely say that is the single biggest stumbling block for ultrasound contrast agents," said Flemming Forsberg, Ph.D., professor of radiology at Thomas Jefferson University and head of research at Jefferson Ultrasound Institute in Philadelphia.
Whether -- or how soon -- the FDA changes its stance is unknown, but the American Institute of Ultrasound in Medicine (AIUM) stepped up its pro-contrast-enhanced ultrasound campaign on March 9 by presenting an educational program for FDA staff. About four dozen healthcare professionals and agency members attended the forum.
"One of the reasons we wanted to look into the approval issue was because ultrasound is not as hot an item as it used to be in radiology," said AIUM President Dr. Lennard D. Greenbaum. "We feel the introduction of contrast agents would greatly stimulate interest in ultrasound among radiologists and hopefully revitalize research and papers in ultrasound."
Following the session, the FDA asked the AIUM to develop guidelines for a clinical study on contrast-enhanced ultrasound. The organization plans to assemble a committee over the next couple of months to discuss the feasibility of such guidelines. "It is very early on; it is a work-in-progress," Greenbaum said. "There is very encouraging interaction with the FDA ... but we are a long way off and there is still a lot of work to do."
FDA concerns
One FDA question, Greenbaum said, is how well contrast-enhanced ultrasound performs on different manufacturers' systems.
"The goal is that an ultrasound contrast agent can be used with any brand of ultrasound machine, as long as it has certain software that will allow for the optimization of visualizing the contrast agent," he said.
Another FDA concern is patient safety with the use of high mechanical index (MI) to burst microbubbles to create the ultrasound image. The FDA fears that high MI could cause premature ventricular contraction and potentially damage tissue in the heart muscle.
While Thomas Jefferson University's Forsberg noted that vessels can rupture if contrast agent microbubbles burst at the wrong time, the problems are caused by ultrasound pressure fields that are much stronger than what is normally used in diagnostic procedures.
"They used dosages or bubbles that are 100 times bigger than what we inject in humans, so that (concern) is not very relevant," he added. "Contrast agents have been injected into hundreds of thousands of patients with remarkably few complications."
Another key to FDA clearance may be how well contrast-enhanced ultrasound's outcomes compare with CT and MR. One demonstration of contrast-enhanced ultrasound's efficacy was exhibited in a study presented in March at the European Congress of Radiology (ECR) in Vienna.
The research compared low MI, real-time contrast-enhanced ultrasound with conventional B-mode ultrasound and 64-slice CT in detecting hepatic metastases from gastrointestinal tumors. The study reviewed 88 patients with known hepatic lesions.
The University of Rome "La Sapienza" study found that the addition of contrast-enhanced ultrasound "improved sensitivity for the detection of individual metastases from 60% to 95%" and was "significantly more accurate than baseline US, especially for small metastases (p < 0.001) with no statistical difference if compared with 64-row spiral CT."
Contrast-enhanced ultrasound also showed more metastases than CT in seven patients, while CT found more lesions than contrast-enhanced ultrasound in two of 22 patients.
Economic benefits
The report shows both clinical promise for contrast-enhanced ultrasound, as well as a less expensive -- and more portable -- imaging option to CT and MR with equally beneficial patient outcomes.
"If you can visualize, for example, organs or the tissue in an abdomen, theoretically, you may not have to do a CT or MR. You just saved $500, $600, or $1,000," said Gordon Parhar, director of Toshiba America Medical Systems' ultrasound business unit. "There is so much talk about reducing spiraling healthcare costs. If we can do that, I think the FDA would be more than willing to listen."
That sentiment was echoed by AIUM CEO Carmine Valente, Ph.D., who said the association would "love to convince the insurers that they are reimbursing for ultrasound that is, perhaps at times, more cost-effective than reimbursing for other more expensive procedures."
Ultrasound also offers safety advantages, Forsberg said.
"You also can argue that doing repeat 64-slice CT scans on a liver is fine, but every time you do it, you load the patient with radiation," he added. "If you can avoid it, all the better."
Elsewhere in the world
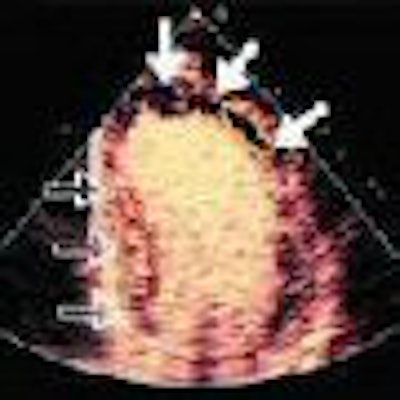
Dr. Roxy Senior, director of cardiac research at Northwick Park Hospital in Harrow, U.K., has researched contrast echocardiography for the last 12 years. Outside the U.S., contrast echo is employed to image the left ventricular cavity, as well as microvessels and capillaries in the heart.
"It is very important to see the myocardial capillaries using contrast, because it gives us objective evidence of myocardial perfusion, in terms of the blood flow and volume of the microvasculature," Senior said. "There is no other technique today that can assess myocardial perfusion by looking at its components as it is done with contrast echocardiography."
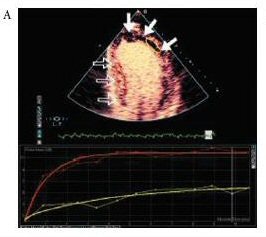 |
| Patient who sustained an anterior myocardial infarction. A Top (above): Apical two-chamber view on MCE after contrast agent injection (SonoVue, Bracco, Milan, Italy) with absence of contrast opacification (solid arrows) at the apex and anterior wall, which were akinetic. The normal, remote segments (outlined arrows) show normal contrast intensity. A Bottom: Replenishment curves in the akinetic segment (yellow) demonstrate very low microbubble velocity and myocardial blood flow remote, normal segment (red). B (below): The corresponding image on CMR demonstrates TEI > 75% in the akinetic segments compared to remote normal remote segment. Images courtesy of Bracco and Dr. Roxy Senior, Northwick Park Hospital, Harrow, U.K. |
 |
Senior believes that contrast-enhanced ultrasound is also likely to become the standard to accurately assess heart function, surpassing MR's high-resolution capabilities, because "contrast ultrasound competes with (MR) almost on an equal footing right now." While cardiac CT views heart structure, CT has yet to develop an effective way to image myocardial perfusion, again making contrast-enhanced ultrasound unique, he said.
In Europe, contrast-enhanced ultrasound is the first examination requested for patients with suspected or known liver disease. Dr. Riccardo Lencioni, from the division of diagnostic and interventional radiology at the University of Pisa in Italy, said the information is used for screenings and follow-up in patients at risk of developing a malignant liver tumor, improving the ability to make a reliable diagnosis.
"In liver cancer, there is a proven ability to make an early diagnosis of cancer and for monitoring ablation procedures," Lencioni added. "Another important area is the assessment of vessels in vascular studies, from transcranial Doppler to renal arteries to any situation in which you have tiny vessels. The use of contrast agents is facilitating the identification of the vessel."
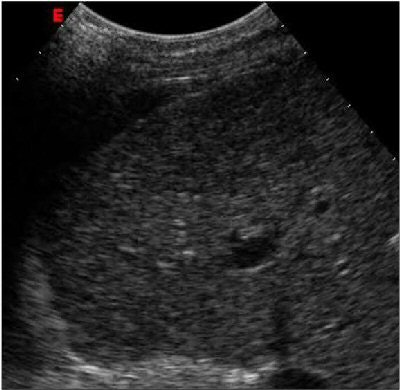 |
| Above: Ultrasound study of an early-stage hepatocellular carcinoma. At baseline examination, the lesion is iso-hypoechoic and hardly detectable. Below: After injection of the contrast agent SonoVue (Bracco), the tiny nodule clearly stands out against the surrounding liver parenchyma due to its arterial vascular supply. Images courtesy of Bracco and Dr. Riccardo Lencioni, University of Pisa, Italy. |
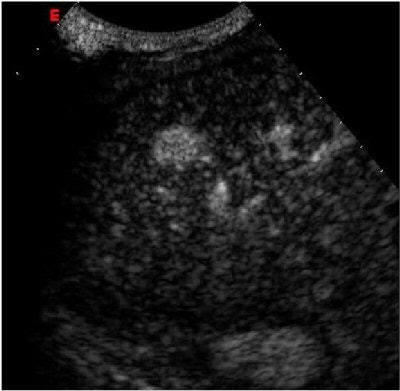 |
Filling the void
Contrast-enhanced ultrasound also appears to be a safer option for patients who may have an adverse reaction to a CT scan with contrast or patients with pacemakers who cannot undergo an MRI scan.
"It is very effective in difficult cases when we cannot decide what to do with studies like CT or MRI or angio," said Dr. Yuko Kono, assistant clinical professor in medicine at the University of California, San Diego (UCSD). "We can detect very tiny arteries or a small flaw. We can tell with much more confidence that there is a thrombosis. It can eliminate an angiography or send the patient for an operation."
Kono agrees with colleagues who believe the FDA's "hurdles are really high" for clearance of contrast-enhanced ultrasound's use in radiology, adding that it would be impossible to prove that the modality is always better than MR and CT.
"(Ultrasound) is a different modality; it will never replace CT or MR," she said. "We can help in different areas, but you can't really compare different modalities like that."
On the horizon
What gives ultrasound so much future potential is the "ability to repeat the procedure hourly or daily, the fact that it's an affordable technology to buy and inexpensive to use, and it's portable," said Don Black, head of R&D for GE Healthcare's medical diagnostics unit. "New, smaller models are being developed, it doesn't involve radiation, and it is noninvasive. Where exactly it will go, we can't be sure, but there are many possibilities, especially intra-abdominal and intravascular applications."
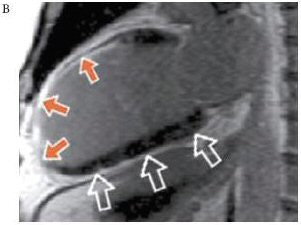
Other future applications for contrast-enhanced ultrasound include the detection of coronary artery disease, coronary blood flow in diabetics, and hypertension. It also could show the amount of myocardium lost due to a heart attack.
 |
| Above: Unenhanced echocardiogram. Below: Echocardiogram enhanced with Definity (Bristol-Myers Squibb Medical Imaging, North Billerica, MA). Image courtesy of Bristol-Myers Squibb Medical Imaging. |
 |
Therapeutic applications could benefit with drug molecules attached to the surface of microbubbles for injection and imaging of the microbubbles in a specific area of the body.
"Under ultrasound, the microbubbles resonate and burst, which gives off the drugs, delivering what it is required to deliver in high concentration," said Northwick's Senior. "It is in the very early stages of development. It has not been used clinically. We are talking five to 10 years time before it is used."
Before any of that promise can be realized in the U.S., however, ultrasound contrast must first gain ground at the FDA.
By Wayne Forrest
AuntMinnie.com contributing writer
April 18, 2006
Related Reading
CEUS aids differentiation of small liver lesions, April 3, 2006
Detection of liver metastases with contrast-enhanced ultrasound, March 23, 2006
Contrast-enhanced US useful for differentiating focal liver lesions, January 19, 2006
Contrast-enhanced ultrasound aids in grading liver disease, December 1, 2005
Copyright © 2006 AuntMinnie.com