VIENNA - Automated breast ultrasound (ABS) promises improved cancer detection when combined with standard digital mammography, but training is required for radiologists to realize its full clinical potential, according to results from a pair of new studies presented Friday at the European Congress of Radiology (ECR).
"Most of the cancers missed by mammography will be found by automated whole-breast ultrasound [AWBU]," said Dr. Kevin Kelly of the Huntington Hill Breast Center in Los Angeles.
"The performance of all readers in this study improved from using mammography alone to mammography plus AWBU -- however, there is considerable variability in breast ultrasound screening skills between radiologists," he said. "This is a problem that needs to be addressed with teaching specifically tailored to the technique."
His work aimed to evaluate the impact of AWBU on the diagnostic competence of 12 community radiologists experienced in mammography, after just four hours of training on the 2D automated system. Kelly, inventor of the SonoCine ABS scanner used in the study (and majority stockholder in the company), noted that ABS could be performed successfully on a high-resolution ultrasound scanner.
Reader performance in diagnosing breast cancer in women with high breast density was assessed using mammography alone, and then again with the addition of ABS. Location information was recorded, along with ACR BI-RADS and Digital Mammographic Imaging Screening Trial (DMIST) likelihood ratings.
Average reading time using AWBU was approximately eight minutes, ranging from slightly less than six minutes to almost 13 minutes. Reader performance across the screening modalities was compared using jackknife alternative free-response receiver operator characteristics (JAFROC).
This defines a figure of merit (FOM), reflecting the probability that a cancer on an abnormal image is scored higher than a falsely marked location on a normal image. Higher FOM indicates superior reader performance, similar to ROC analysis.
Enhanced performance
AWBU added to standard digital mammography, versus mammography alone, saw reader-averaged FOM scores improve significantly by BI-RADS (0.783 versus 0.671; p < 0 .001) and likelihood (0.789 versus 0.674; p < 0.001).
Overall, Kelly observed that AWBU plus mammography saw the average performance of every reader in the study improve across the board:
Percentage improvement in breast cancer detection with ABS plus mammography (M)
|
||||||||||||||||||||||||||||||||
"Over the past 30 years, there has been considerable debate about screening breast ultrasound, but now AWBU has given us a standardized method for testing ultrasound as an adjunct to mammography," Kelly noted.
Discrepancy between readers
However, the study also revealed considerable variation in skill between breast radiologists when using AWBU. Kelly deemed the degree of inconsistency as unacceptably extensive, a feature highlighted also by a separate new, Norwegian study presented at ECR.
"ABS as adjunct to mammography in screening should be performed by the same radiologist that interprets the original mammogram," asserted Dr. Per Skaane, of Ullevaal University Hospital in Oslo.
His team examined 114 breasts using digital mammography (Senographe D/DS, GE Healthcare, Chalfont St. Giles, U.K.) and a 3D ABS system (SomoVu, Siemens Healthcare, Erlangen, Germany).
Five radiologists experienced in breast imaging using BI-RADS assessment categories 1-5 interpreted the images, using ABS alone at first reading; this was followed by ABS plus mammography six weeks later. Reader performance was assessed with ROC analysis.
Echoing the findings from Kelly's study, Skaane too observed universal improvement in reader competence for diagnosis of breast cancer through combined ABS-mammographic interpretation, though the degree of improvement between readers was significant.
|
Sensitivity varied from 50% to 97% and specificity ranged between 33% and 96%.
"ABS is a promising technology," he noted. "However, there was considerable interobserver variability" -- which he accounted for through differences in the interpretation environment, ABS reading protocol, and the learning curve.
ABS versus handheld ultrasound -- first results
A third new study presented on Friday reported preliminary results from a comparison of ABS with a more traditional handheld ultrasound device for breast cancer identification and diagnosis.
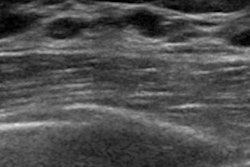
A team led by Dr. Dirk Clevert of the University of Munich in Germany compared lesion visibility in 53 breasts between March and May 2009 using ABS (Acuson S2000 ABVS, Siemens Healthcare, Erlangen, Germany) with images acquired using a handheld ultrasound device with a 13-MHz transducer (Acuson Antares, Siemens). All lesions were classified according to BI-RADS assessment.
The handheld ultrasound device depicted 25 lesions in 17 of a total 27 patients, which were confirmed by the ABVS. Lesion size ranged from 5 to 35 mm (median, 17 mm). Median scanning time for the ABVS was 8.2 minutes for each breast, with interpretation time spanning three to 18 minutes.
The ABVS found all breast cancers, and there was good agreement regarding BI-RADS classification with the handheld method.
Based on these initial findings, Clevert suggested that ABVS imaging allows "detection of solid and cystic lesions and their BI-RADS classification with a high reliability," in comparison to handheld ultrasound.
In summary, the three new studies appear to align in their findings that automated breast ultrasound scanning can improve breast cancer detection and diagnosis, whether added to standard digital mammography or as a standalone modality.
The challenge surrounding ABS lies in the implementation of bespoke training for radiologists on its use during breast scanning, with the aim of achieving greater consistency between readers and translating the enhanced performance into tangible clinical benefits.
By Rob Skelding
AuntMinnie.com contributing writer
March 5, 2010
Related Reading
Targeted breast US stands on its own for women under 30, December 24, 2009
Ultrasound breast scanning protocol boosts efficiency, June 3, 2009
Future of ultrasound will require technology, educational gains, April 4, 2009
Automated breast US unit not ready to replace handheld, study finds, March 16, 2009
Siemens' RSNA launches span CT, MRI, x-ray and US modalities, November 27, 2007
Copyright © 2010 AuntMinnie.com