Ultrasound elastography can be a useful problem-solving tool for assessing focal prostate lesions detected on transrectal ultrasound, potentially avoiding the need to biopsy some patients, according to research published in the May issue of the Journal of Ultrasound in Medicine.
In a study of almost 70 patients, a team from Seoul National University Bundang Hospital found that biopsying focal lesions with certain criteria -- those with suspicious characteristics on transrectal ultrasound and also having strain measurements above a defined cutoff value on elastography -- would yield over 75% sensitivity and over 90% specificity for diagnosing cancer.
"Any focal lesion on [transrectal ultrasound] with a strain index of 2.4 or more is at risk for prostate cancer," said co-author Dr. Hak Jong Lee "If the focal lesion is [also] located in the outer half of the peripheral zone, its outline is irregular, its shape is nodular or clustered low-echoic, and it is hypervascular on [color Doppler ultrasound], the possibility of cancer is much increased and an added biopsy for this lesion might be necessary."
An emerging modality
While transrectal ultrasound has traditionally been the primary imaging modality for the prostate, it suffers from the limitations of low sensitivity and a lack of reader agreement. The addition of color Doppler has been reported to increase cancer detection rates, but the combination of color Doppler and grayscale ultrasound still isn't sufficient for diagnosing prostate cancer, according to the group (J Ultrasound Med, May 2016, Vol. 35:5, pp. 899-904).
 Dr. Hak Jong Lee from Seoul National University Bundang Hospital.
Dr. Hak Jong Lee from Seoul National University Bundang Hospital.Ultrasound elastography, however, has shown promise and been reported to improve prostate cancer detection. The majority of research studies involving elastography in the prostate have assessed the overall accuracy of the technique in comparison with systemic biopsy, but the Seoul National University team elected to focus on the role of elastography as an adjunctive or problem-solving method when encountering suspicious lesions on ultrasound alone.
"We hoped that elastography can help to decide whether this suspicious lesion should be biopsied or not," Lee told AuntMinnie.com.
The study included 69 patients with focal lesions that were found on transrectal sonography. The individuals were referred for transrectal ultrasound-guided prostate biopsy between June 2012 and August 2013. A uroradiologist with 14 years of experience performed all transrectal ultrasound and elastography studies on a Logiq E9 ultrasound scanner (GE Healthcare) with a 5- to 9-MHz multifrequency endocavitary probe.
Based on the institution's criteria related to the lesion location, outline, shape, and vascularity on color Doppler, the focal lesions were initially classified as either highly suspicious or less suspicious for cancer.
Lesions were considered highly suspicious for cancer if they had the following features on transrectal ultrasound:
- The lesion was located in the outer half of the peripheral zone of the prostate.
- The lesion had an irregular outline.
- The lesion's shape was nodular or clustered low-echoic.
- The lesion was hypervascular on color Doppler ultrasound.
The uroradiologist used a sector transducer to perform elastography for the patient's most suspicious focal lesion. The lesion's strain index was automatically calculated by dividing the strain ratio of a normal-looking area of tissue by the strain ratio of the focal lesion. All patients then received systematic 12-core randomized biopsies as well as two targeted biopsies. Of the 69 patients, 31 (44.9%) were found to have prostate cancer.
The researchers then compared the elastography strain indices with the biopsy results. Strain indices by lesion type were as follows:
- Malignant lesions: 3.26 ± 1.77 (range, 0.40-8.47)
- Benign lesions: 2.16 ± 1.52 (range, 0.15-6.40)
The difference was statistically significant (p = 0.008).
A winning combination
Lee and colleagues set a strain index value of 2.4 as the cutoff for determining malignancy; lesions with values higher than this were more likely to be cancerous. Combining the strain index value with the classification of lesions as highly suspicious proved to offer the best performance.
| Performance for differentiating prostate lesions | ||
| Sensitivity | Specificity | |
| Elastography strain index cutoff value of 2.4 and classification as highly suspicious on transrectal ultrasound | 76.5% | 92.9% |
| Elastography strain index cutoff value of 2.4 | 66.7% | 71.1% |
| Classification as highly suspicious on transrectal ultrasound | 70.8% | 68.9% |
"This cutoff value of 2.4 for the strain index looks to be useful, especially when an examiner encounters highly suspicious focal lesions on transrectal sonography, as this value can provide guidance with regard to suggesting a biopsy," the authors wrote.
In other study findings, the strain index had a moderate linear correlation with the lesion Gleason scores (r = 0.441; p = 0.013).
"This finding may be attributed to the fact that prostate cancer with a higher grade has a higher cell density and tends to be stiffer," the authors wrote.
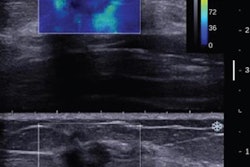
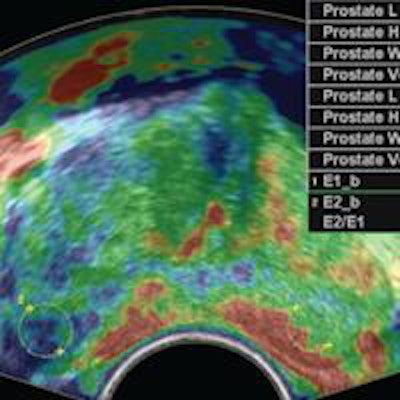
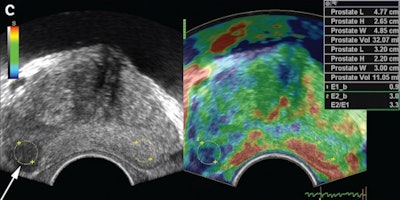 Elastogram from a 71-year-old man with prostate cancer in the peripheral zone that was classified as a highly suspicious focal lesion on transrectal sonography. Elastogram shows higher stiffness (blue) at the lesion (arrow). Each region of interest had an area of 0.31 cm2 and was located 0.2 mm from the outer margin of the prostate. The lesion had a strain index of 3.3 and the area was confirmed as prostate cancer with a Gleason score of 9. Image courtesy of the Journal of Ultrasound in Medicine.
Elastogram from a 71-year-old man with prostate cancer in the peripheral zone that was classified as a highly suspicious focal lesion on transrectal sonography. Elastogram shows higher stiffness (blue) at the lesion (arrow). Each region of interest had an area of 0.31 cm2 and was located 0.2 mm from the outer margin of the prostate. The lesion had a strain index of 3.3 and the area was confirmed as prostate cancer with a Gleason score of 9. Image courtesy of the Journal of Ultrasound in Medicine.Based on the research results, the hospital is now utilizing this approach clinically.
"We currently measure strain index when a suspicious lesion is encountered in either routine ultrasound exam or prebiopsy ultrasound scans," Lee said. "If the index is over 2.4, additional biopsy for the focal lesion will be [performed]."