It's standard practice to perform imaging surveillance of thyroid nodules found to be benign on biopsy. But this follow-up is expensive and only rarely leads to the detection of thyroid cancer, according to a study published in the February issue of the American Journal of Roentgenology.
A team of researchers from Thomas Jefferson University (TJU) in Philadelphia recently quantified the cost of surveillance imaging and its cancer detection rate in a study of nearly 1,700 patients who had received a benign fine-needle aspiration (FNA) biopsy of a thyroid nodule. Nearly half of those patients received imaging follow-up at an average cost of almost $1,100 per patient.
Thyroid cancer was ultimately diagnosed in just over 2% of these patients, representing a cost of more than $46,000 per cancer detected.
"We believe that the benefits of following biopsy-proven benign thyroid nodules do not merit the considerable costs associated with this practice, especially when considering overdiagnosis and highly favorable outcomes for papillary thyroid carcinoma," wrote the team led by Dr. David Becker-Weidman, now at Beth Israel Deaconess Medical Center in Boston (AJR, February 2017, Vol. 208:2, pp. 358-361).
Overdiagnosing and overtreating?
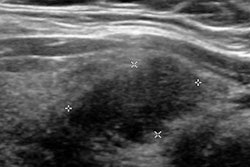
Thyroid nodules are very common, and thyroid imaging volume has substantially increased over the past 20 to 30 years, Becker-Weidman said. Separate guidelines published by the American Thyroid Association (ATA) and the American Association of Clinical Endocrinologists (AACE) recommend follow-up ultrasound and ultrasound-guided FNA for these nodules based on differing criteria.
But neither of the guidelines offers any recommendations on when or if ultrasound surveillance can be discontinued for a stable nodule, according to the researchers.
"The incidence of thyroid cancer has ... significantly increased while the mortality rate has remained relatively unchanged," Becker-Weidman told AuntMinnie.com. "This suggests that we are overdiagnosing and overtreating clinically insignificant cancers. [In addition], none of the major clinical guidelines specify an end point for following biopsy-proven benign nodules, so many patients receive yearly ultrasound ad infinitum."
As a result, the researchers wanted to quantify the cost of imaging follow-up after a benign biopsy to inform future discussions about cost-effectiveness in the era of accountable care organizations. Using their institutional pathology database, they identified all patients who had a benign thyroid FNA biopsy at Thomas Jefferson University Hospital between January 1, 1999, and December 31, 2003.
They then gathered subsequent information on imaging tumor surveillance and cancer detection by searching the patients' electronic medical records. The researchers also calculated cost information by using the facility's total relative value unit (RVU) and the 2014 Hospital Outpatient Prospective Payment System conversion factor.
Of the 1,685 patients who had a benign thyroid biopsy over that five-year period, 800 (47.5%) received follow-up imaging. Thyroid ultrasound was the most common follow-up study.
| Cost of thyroid follow-up by imaging modality | ||
| Modality | No. of studies | Cost |
| Thyroid ultrasound | 2,223 | $529,874 |
| Ultrasound-guided thyroid FNA biopsy | 606 | $176,157 |
| Neck CT | 78 | $39,622 |
| Neck MRI | 53 | $53,114 |
| Total | 2,960 | $879,347 |
Low yield
The total imaging cost reached $879,347, or $1,099 per patient, according to the researchers. Over a mean follow-up period of 7.3 years, the patients received a mean of 3.9 follow-up imaging examinations (range, 1-17). Only 19 (2.4%) of these patients were diagnosed with thyroid cancer in the follow-up period, including 17 (89.5%) cases of papillary carcinoma and two (10.5%) cases of Hurthle cell carcinoma.
Those cancer diagnoses came at a cost of $46,281 per patient, according to the group.
What's more, the "cost analysis greatly underestimates the total cost to the patient and healthcare system because we only examined the cost of surveillance imaging at a single institution," they wrote. "We did not include the cost of office visits to an endocrinologist, surgical consultations, surgical procedures, or imaging examinations performed at other institutions."
The authors acknowledged limitations of their study, including its reliance on the experience of a single, large urban teaching hospital. In addition, half of the patients did not receive follow-up imaging at the institution and presumably received their care elsewhere, according to the group.
"Although these circumstances are not ideal, they will not affect costs calculated on a per-patient or per-cancer basis," they wrote. "In addition, because the demographic information of the patients who received follow-up is similar to that of all patients with a benign biopsy, selection bias likely did not significantly affect our results."
Perpetual follow-up
The TJU team noted that clinicians are obligated to recommend perpetual follow-up of thyroid nodules because of medicolegal concerns, as well as the lack of clear end points in the clinical guidelines provided by the American Thyroid Association and the American Association of Clinical Endocrinologists.
"Management is also complicated by the possibility of a false-negative examination and the fact that interval growth is used as a surrogate marker for malignancy," they wrote. "This approach is questionable because many benign nodules will increase in size over time, which prompts additional biopsies, surgical procedures, or both."
Despite their findings, the authors don't recommend a change in how these patients are managed.
"Any change in management must originate from the endocrinologists and [primary care physicians] who are ordering these imaging exams and the major endocrinology associations that publish clinical practice guidelines," Becker-Weidman said. "We hope that our study provides useful information to those groups that set national and institutional policies in an era of relatively scarce resources."
Becker-Weidman and colleagues are continuing to study this topic: In the next phase, they will seek to determine the benefit that patients receive by undergoing postbiopsy imaging, he said.